ALLERGIC RHINITIS (AR) - Seasonal, perennial and occupational


Overview
What's happening?
- Expelling an allergen. Induces sneezing, watery/itchy eyes, and runny nose.
- Preventing more of the allergen from entering the body. Increases mucus production and swelling of the nasal passages.
During an allergy attack, antibodies, usually immunoglobin E (IgE) attach to IS cells, including histamine-releasing basophils in circulation and mast cells in the lungs, skin, and mucous membranes. When IgE antibodies bound to I.S. cells encounter antigens (called allergens when involved with allergies), the IS cells are prompted to release chemicals that injure surrounding tissues. One chemical released is histamine, which opens the blood vessels causing skin redness and swollen membranes. In the nose, this manifests as sneezing and congestion
- Typical allergens include. Plant pollens, some fungi, house plants, mold spores / mildew, dust mites, animal dander, industrial chemicals (including tobacco smoke), foods, medicines, and insect venom.
- Affects people of all ages. An estimated 30% of Westerners
- SEASONAL allergic rhinitis (better known as “Hay fever”). Affects > 23 million Americans annually. Tree, grass and weed pollens, and some airborne mold trigger seasonal allergic nose and eye allergy during springtime and early summer. Seasonal allergic rhinitis symptoms include nasal and eye itching with explosive sneezing, watery eyes and nose and itchy palate and ears, with profuse postnasal drip . Seasonal allergic rhinitis patients do not develop the typical “allergy face” but have seasonal puffiness of the eyes and eyelids with associated nasal membrane swelling.
- PERENNIAL allergic rhinitis. Usually caused by indoor allergens such as house dust mites and pet skin flakes . Perennial allergic rhinitis is similar to hay fever, in that the allergen causes inflammation and irritation of the delicate linings in the nose and eyes. However, the allergic rhinitis goes on throughout the year as opposed to seasonal allergic rhinitis which occurs only during certain seasons.
- OCCUPATIONAL allergic rhinitis. Reaction to particles in the work environment. Such as grain dust or animal dander (agricultural workers), sanding / cutting materials (construction workers), adhesives (construction, manufacturing), chemicals used in a hair salon, flour in a bakery
More specific "goings-on" with AR
In most cases, AR is an allergic reaction to a specific allergen in the nasal mucosa. The allergen binds to the immunoglobulin E (IgE) antibody (specific to the allergen e.g. cat dander) on the surface of the immune system mast cell, which initiates:
- Initial-Response Phase – Recruitment of numerous chemo-attractants and inflammatory mediators, which signal infiltration of eosinophils, basophils, neutrophils, and monocytes.
- Delayed-response phase (~2-8 hours after exposure)-inflammatory mediators in tissue lead to damage of mucosal epithelial cells. This phase is associated with increased sensitivity to allergens after repeated exposure and hyper-responsiveness to irritants.
Mast cells – are found in high concentrations in blood vessels of the sub-epithelial connective tissue of the respiratory tract and conjunctiva. Mast cell degranulation (release of active substances) accounts for ~ half AR symptoms.
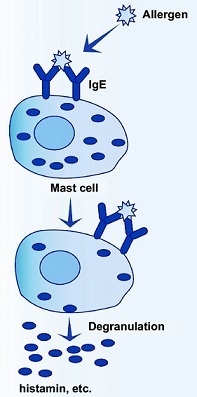
HISTAMINE (main inflammatory mediator in AR) – is released by mast cells in the immediate-response phase and basophils in the delayed-response phase. When histamine binds to H1-receptors, it increases vasodilation, capillary permeability and smooth muscle contraction, resulting in rapid fluid leakage into nasal tissues and swollen, secretory nasal linings.
Evans R III. Epidemiology and natural history of asthma, allergic rhinitis, and atopic dermatitis. In: Middleton E Jr, Reed CE, Ellis EF, et al, eds. Allergy Principles and Practice 4th ed. St. Louis, MO: Mosby; 1993:1109-1136.

Symptoms of allergic rhinitis
Symptoms of allergic rhinitis may develop within minutes after breathing in an allergen, or sometimes hours later – The most common immediate allergic rhinitis symptoms include:
- Repeated sneezing. Can occur upon waking in the morning (especially during hayfever season).
- A runny nose. Drainage from a runny nose caused by allergies is usually clear and thin but may thicken and become cloudy or yellowish if a nasal or sinus infection develops.
- Postnasal drip. Feels like a tickle in your throat and can trigger a cough as you try to clear your throat. AR is the most likely cause of postnasal drip.
- Watery, itchy eyes. Also, itchy ears, nose, and throat can present as symptoms.
- Significant sleep disturbance seen in those with severe symptoms. Compared to people with mild allergic rhinitis. People with allergic rhinitis use significantly more sleeping pills and alcohol than those with clear noses.
Archives of Internal Medicine, September 2006.

Causes of allergic rhinitis
Predisposing factors
These include a family history of similar symptoms and a personal history of eczematous dermatitis, urticaria, and/or asthma.
Likely causes
The most blamed culprit is the allergen to which the immune system is over-reacting. However, since some people are not affected by AR we should look to other explanations:
Lifestyle
A study of nearly 4,300 German adults found that those whose partners had hay fever were at greater risk of developing such allergies themselves, and the longer couples lived together, the higher the hay fever risk climbed. The authors of the study published in the journal Allergy say the findings point to the importance of environment and lifestyle in the risk of developing allergies, since cohabitating couples have many of these factors in common.
Diet
AR can be the consequence of not having an immune system that has a controlled, as opposed to overzealous response to allergens, which requires:
- A balance of anti-inflammatory and inflammatory essential fats. In particular, there is a general excess of inflammatory omega-6 fatty acids typically found in grocery store oils and processed foods, and used in restaurants.
- An adequate supply of antioxidants to combat reactive oxygen species (ROS) produced during the inflammatory process. Chronic inflammation can damage healthy tissue (called oxidative stress). Combative antioxidants would include:
- Vitamins A, B,C, E and flavonoids (E.g. quercetin). Found in fruits and vegetables and supplements;
- VITAMIN D. Produced in skin exposed to sunlight. VITAMIN D levels are lower in children who have allergies.
- MELATONIN. Hormone produced in the body during a good night’s sleep
- Others. E.g. supplemental CoQ10.
“In-house” antioxidants SOD, CAT, and GPx. Produced by body, but require antioxidant support nutrients including copper, iron, manganese, selenium and zinc.
Many of those with AR also have allergy symptoms triggered by substances in certain foods. E.g. eggs, nuts, fish, shellfish, dairy products or wheat. Early food allergies seem to be the strongest predictor of subsequent allergic disease. PubMed














