Peripheral Neuropathy (PN) - Damage to nerves affecting brain communication with our body
Overview
Neuropathies affect at least 20 million people in the U.S.
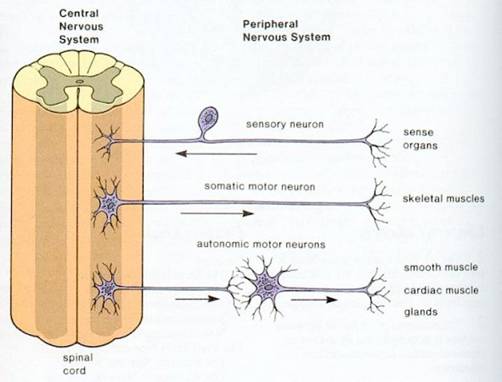
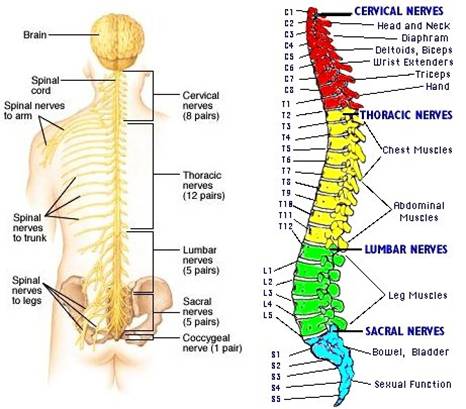
Peripheral nerves branch out of the spinal cord to all parts of the body – providing communication pathways between the central nervous system (CNS), i.e. the brain and spinal cord, and the muscles, skin, internal organs, and blood vessels. Damage to this communication network can cause the equivalent of static on a phone line and is called peripheral neuropathy or neuropathy.
PN commonly starts in the longest nerves. i.e. those going to your toes;
PN may affect one to several nerves:
- Mononeuropathy. 1 nerve;
- Multiple mononeuropathy. 2 or more nerves in different areas;
- Polyneuropathy. Many nerves.
Neuropathy is also classified by its cause or location – these include:
- Diabetic neuropathy
- Nutritional neuropathy
- Radiculopathy. Neuropathy resulting from pressure on / injury to a spinal nerve root (Radix) affecting nerve function. Radicular pain and other symptoms (weakness, numbness, pins and needles, lack of muscle control) may manifest as “referred” pain / symptoms in an extremity. E.g. Impingement in the lower back can result in pain/symptoms in the foot. Radiculopathy may be experienced in such as herniated disk, spinal stenosis (narrowing of spinal canal), sciatica and degenerative disk disease.
- Entrapment neuropathy. Occurs when inflammation of connective tissue puts pressure on a nerve
passing through it. - Idiopathic neuropathy. When a cause cannot be identified.
See Peripheral nervous system 101 for some simple, informative diagrams
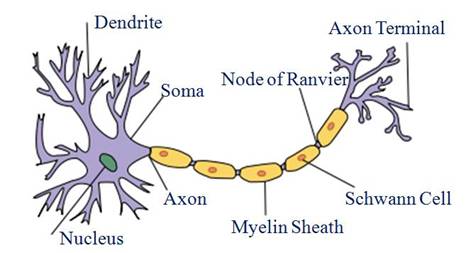
Damage specifically occurs to axons or myelin surrounding peripheral nerves. The axon is the “fiber-optic cable” of a neuron for transmitting messages from its neuron body (soma) to make contact with other cells – usually neighboring neurons but sometimes muscle or gland cells.
Types of peripheral neuropathy
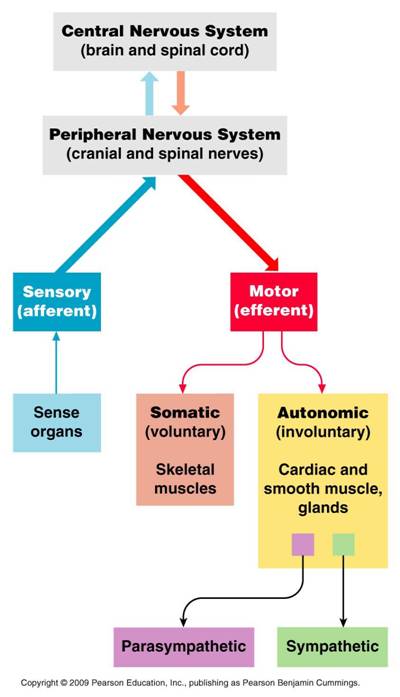
(1) Motor (efferent) neuropathy
Affects nerves sending messages from the brain for voluntary / conscious control of muscles for movement (part of the somatic nervous system (SNS) ).
Damaged motor nerves may:
- Impair movement and can lead to muscle weakness / wasting or even paralysis
(2) Sensory (afferent) neuropathy
Also part of the SNS, it affects nerves that receive and transmit sensations from parts of the body to the brain, E.g. heat, pain or touch.
Damaged sensory nerves may:
- Stop relaying signals. Resulting in numbness and pain (most often in hands and feet)
- Send incorrect signals. Transmitting sensations of pain, burning or tingling sensations (sometimes
described as “pins and needles”)
(3) Autonomic neuropathy
Controls subconscious (involuntary) functions of sensory and motor nerves affecting body’s housekeeping – of such as blood
pressure, heart rate, digestion and bladder function; (part of the autonomic nervous System (ANS) )
Damaged autonomic nerves may:
- Impair any involuntary function – depending on location of damage and can be serious.
Symptoms of peripheral neuropathy (PN)
Symptoms vary depending on type of nerves affected and may include:
- Gradual onset of numbness and tingling in feet or hands. May spread upward into your legs and arms
- Burning / Searing pain. Especially at night, when it can seriously disrupt ability to sleep
- Sharp, jabbing or electric-like pain
- Extreme sensitivity to touch. Even light touch
- Lack of coordination
More severe cases experience:
- Muscle weakness / wasting or paralysis, if motor nerves are affected
- Autonomic nerve dysfunction (Organ / gland dysfunction)
With an inability to:
- Swallow / digest food properly and / or control bowel function. Lack of esophageal or intestinal muscle control (possibly manifesting as diarrhea or constipation)
- Maintain healthy blood pressure. Lack of arterial muscle control for contraction/dilation -experienced as dizziness, lightheadedness, or even fainting when a person moves suddenly from a seated to a standing position
- Control bladder function. Lack of bladder muscle control can cause incontinence, retention or lead to infection
- Sweat normally
- Have normal sexual function
Causes of peripheral neuropathy
Numerous factors can cause neuropathy damage with inherent inflammation
Autoimmune diseases. E.g. Lupus, rheumatoid arthritis and Guillain-Barre syndrome. Some neuropathies are caused by inflammation resulting from immune system activities and can develop quickly or slowly.
- Acute inflammatory demyelinating neuropathy (aka Guillain-Barre syndrome). Can quickly damage motor, sensory, and autonomic nerve fibers; Most people recover from this syndrome although severe cases can be life threatening.
- Chronic inflammatory demyelinating polyneuropathy. Usually damages sensory and motor nerves, but not autonomic nerves; can alternate between remission and relapse.
- Acute or chronic multifocal motor neuropathy. Affects only motor nerves.
Diabetes (Diabetic peripheral neuropathy). More than 50% of diabetics develop some type of neuropathy to several nerves; nerve endings slowly die leading to loss of sensation in the feet, legs and hands which at times can be painful and can lead to weakness and difficulty walking. Nerve damage may result from impaired ability to utilize glucose for energy.
Toxin exposure. Can cause peripheral nerve damage:
- Heavy metals. E.g. arsenic, lead, mercury, thallium; Magnesium deficiency allows heavy metal deposition in the brain.
- Certain medications. Certain anti-cancer drugs (especially chemotherapy), anticonvulsants, antiviral agents, and antibiotics.
- Environmental toxins
Infections. Some viral or bacterial infections that can cause peripheral neuropathy by directly attacking and damaging sensory nerves, often producing sharp pain. Viral and bacterial infections can also cause indirect nerve damage by provoking autoimmune disorders. In this case, I.S. components attack the neural myelin sheath or axon.
BACTERIA / VIRUS | ASSOCIATED DISEASE |
Borrelia burgdorferi (spirochete bacteria) | Lymes Disease – rapidly developing, painful polyneuropathy, often within a few weeks after initial infection by a tick bite. |
| Corynebacterium diphtheriae | Diphtheria |
| Mycobacterium leprae / lepromatosis | Leprosy |
| Varicella-zoster | Shingles – Postherpetic neuralgia occurring after an attack of shingles |
| Epstein-Barr virus | Epstein-Barr |
Inherited disorders. E.g. Charcot-Marie-Tooth disease, amyloid polyneuropathy.
Traumatic injury. Can sever / crush / compress / stretch peripheral nerves.
- Motor vehicle accidents
- Falls
- Sports injuries
Pressure on the nerve. Can compress nerve fibers:
- Slipped disks between vertebrae
- Broken/dislocated bones
- Using a cast or crutches / Spending a long time in an unnatural position
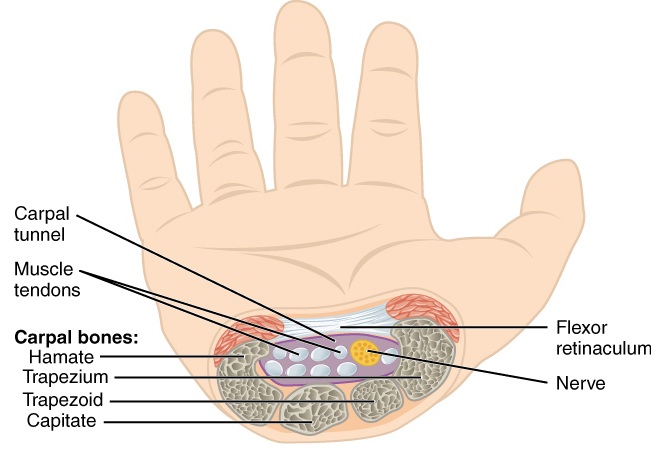
- Repetitive Stress /Repeating a motion many times (E.g. typing) – repetitive flexing of any group of joints for prolonged periods often leads to entrapment neuropathies, by causing ligaments, tendons, and muscles to become inflamed and swollen, constricting the narrow passageways through which some nerves pass. E.g. Carpal tunnel syndrome
- A pinched nerve in the back
- Tumors. Growths can form directly on the nerves themselves, or tumors (malignant and benign) can exert pressure on surrounding nerves contributing to PN;
Acute and chronic inflammation of connective tissue. Acute inflammation of protective tissue surrounding nerves can spread directly into nerve fibers. Progressive destruction of connective tissue from low level chronic inflammation renders nerve fibers more vulnerable to compression injuries and infections. Inflamed, swollen joints can entrap nerves, with ensuing pain.
Vitamin deficiencies / Alcoholism. Vitamins B1 (thiamine), B3 (niacin), B6, B12, E are particularly important to nerve health and whose deficiency is a factor in PN.
B1 deficiency is typically seen in alcoholics
There are several causes of B12 deficiency:
- A strict vegetarian diet. Since animal-based foods such as red meat, dairy products, fish, poultry and eggs are the only recognized source of dietary B12.
- Inability of stomach acids to aid in B12 absorption. As such, drugs taken to reduce stomach acid should be taken with B12 supplements.
- Other conditions/procedures associated with a reduced ability to absorb B12. Include autoimmune diseases, pernicious anemia, pancreatic diseases, ileal resection, Crohn’s disease, HIV infection, gastritis, gastric or small intestine surgeries, malabsorption syndromes, M.S.
Kidney disease, liver disease. By allowing abnormally high amounts of toxic substances in the blood that can severely damage nerve tissue. Most patients on dialysis because of kidney failure develop polyneuropathy.
Reduced oxygen supply to peripheral nerves. Hypoxia caused by vascular damage or diseases of the blood can seriously damage or kill nerve tissue. Blood flow is impeded as blood vessels become inflamed, which reduces lumen size as vessel walls harden, thicken, and develop scar tissue. Blood vessel constriction is often present with diabetes.
Hormonal imbalances. Can disturb normal metabolic processes and cause neuropathies.
- Underproduction of thyroid hormones (Hypothyroidism). Slows metabolism, leading to fluid retention and swollen tissues that can exert pressure on peripheral nerves.
- Overproduction of growth hormone. Can lead to acromegaly, a condition where many parts of the skeleton become abnormally enlarged. Nerves running through enlarged joints can become entrapped.
- Estrogen neuropathy. In women, neuropathy can start within a decade of approaching menopause. Search for: “Estrogen Neuropathy”, “Menopause Neuropathy”, “Hypothyroidism Neuropathy”
Gluten sensitivity. PN may respond to a strict gluten-free diet
M Hadjivassiliou et al, Sensory ganglionopathy due to gluten sensitivity. Neurology. 2010 Sep 14;75(11):1003-8. PubMed
M Hadjivassiliou et al, Neuropathy associated with gluten sensitivity. J Neurol Neurosurg Psychiatry. 2006 Nov;77(11):1262-6. Epub 2006 Jul 11. PubMed
3-step treatment for peripheral neuropathy

The good news
Provided the nerve cell is still alive, peripheral nerve cells have a remarkable ability to regenerate themselves. Symptoms can usually be controlled by various means, but the real cure is to prevent new damage by identifying and eliminating what is causing the neuropathy.

(1) Symptomatic treatments to control inflammation
Natural / alternative symptomatic treatments for neuropathy
General recommendations to counter and control inflammation: INFLAMMATION – Can’t live with it, can’t live without it
Transdermal DMSO
Small scale studies conducted in the early 1980’s suggested DMSO may help to relieve peripheral neuropathy Kingery, 1997
- DMSO has a powerful anti-inflammatory effect
- DMSO is a powerful antioxidant
- DMSO contains sulfur – a component of nerve protecting vitamin B1
DMSO – Carrier and Penetrant / Stop Pain & inflammation
Alpha Lipoic Acid (R-ALA)
Universal fat- and water-soluble antioxidant
R-ALA offers several benefits against peripheral neuropathy
- Alpha Lipoic Acid (a.k.a. thioctic acid or R-ALA) is the key to significant reduction of neuropathy and nerve pain.
- R-ALA is a sulfur-containing fatty acid found inside every cell of the body; the reduced form of α-lipoic acid is dihydrolipic acid (DHLA)
- R-ALA helps generate energy. R-ALA is an essential cofactor for several mitochondrial enzymes critical to cellular energy production. Also found to act similarly to INSULIN by increasing numbers of cell “transporters”(GLUT-4s) that carry glucose into cells and increasing glucose uptake PubMed
- This potent fat- and water-soluble antioxidant can neutralize potentially damaging radicals (both reactive oxygen and nitrogen species) just about anywhere in the body. As can its reduced form DHLA; although supplemented body concentrations are 10-fold less than vitamin C and glutathione and it is quickly eliminated from cells.
- Glutathione (GSH) synthesis. This “in-house” master antioxidant deals with potentially carcinogenic toxins in the body; aging-reduced levels are enhanced by α-lipoic acid
- DHLA (the reduced form of α-lipoic acid) has the unique ability to recharge other fat- and water- soluble antioxidants that have been used up. E.g. Vitamins B, C and E, CoQ10 (important in mitochondrial electron transport chain in cellular energy production) and glutathione; protects microcirculation to the nerves by combating free radicals, a primary cause of nerve damage.
- R-ALA and DHLA are effective chelators of free transition metal iron and copper ions. Preventing them from catalyzing reactions that produce potentially nerve-damaging free radicals.
- Can cross the blood-brain-barrier / Specific effect on nerves eases neuropathy-associated burning, pain, and numbness.
R-ALA is synthesized in the body and a small amount obtained from food. In the cell mitochondria 2 sulfur atoms are inserted into octanoic acid (an 8-carbon fatty acid).
Dosage of R-ALA to counter peripheral neuropathy
- 150 mg R-ALA twice per day or 600-1200 mg /day of a 50/50 mix of R-ALA and S-ALA. Several studies have shown 100% R-ALA (form occurring in food) to be more effective than the cheaper, more commonly used S-ALA. For best bioavailability, take on an empty stomach (one hour before or two hours after eating).
Some scientists’ results using R-ALA for neuropathy
- Researcher L. Androne found that “The antioxidant therapy with R-ALA improves and may prevent diabetic neuropathy.”
- “Treatment with R-ALA over 3 weeks is safe and effective in reducing symptoms of diabetic peripheral neuropathy”. Reports scientist FA Gries.
- “Oral treatment with R-ALA for 5 weeks improved neuropathic symptoms.” Ziegler & Gries, 1997; Kahler et al, 1993; Ziegler et al, 1995; Packer et al, 1995; Ruhnau et al, 1999
- Animal studies have indicated that a combination of ALA with ALC (see below) can actually reverse and repair the neurological and cognitive declines that occur with aging.
Acetyl-L-Carnitine (ALC)
- Amino acid responsible for transporting certain fatty acids into cell mitochondria for energy production.
- 20 years of benefits with Alzheimer’s and cognitive disorders
More recent studies show ALC reduces pain and increases nerve conduction in PN
Italian study published 2002
333 patients with diabetic peripheral neuropathy were randomized in a double-blinded, placebo-controlled fashion. Half of the patients received initial doses of 1000 mg daily of intramuscular ALC for 10 days followed by 2000 mg / day orally for the remainder of the year. At the end of the study, those patients treated with ALC showed a statistically significant improvement in nerve conduction responsiveness compared to placebo. In addition, after twelve months of treatment the ALC group had a statistically significant reduction of pain by 39% compared to 8% in the placebo group. The conclusion was that ALC was effective and well tolerated in improving neurophysiological parameters and reducing pain over a one-year period. It was felt to be a promising treatment option in patients with diabetic peripheral neuropathy.
2010 study published in England
Pre-treating animals with ALC seemed to have a protective effect on peripheral nerves that were then experimentally destroyed. Study authors suggest ALC may be suitable for clinical use in preventing nerve death after peripheral nerve trauma.
N- Acetyl Cysteine (NAC)
- NAC has been shown to be neuroprotective in traumatic brain injury. A potent antioxidant, NAC reduces inflammatory cytokines and proteins, reducing edema. NAC is a precursor to body’s master antioxidant glutathione. Sagara et al, 1996; Love et al, 1996
Transdermal (or intravenous) magnesium
- Reduced magnesium levels can increase acute pain and induce chronic neuropathic pain. Low magnesium levels not only inhibit the body’s capacity to block the NMDA receptor site, contributing to higher levels of acute or immediate pain, but in addition, low magnesium levels make central sensitization of the spinal cord more likely to occur, which can lead to chronic neuropathic pain.
- Magnesium deficiency also allows potentially damaging heavy metal deposition in the brain.
- Take a nightly footbath in a solution of magnesium chloride crystals and water. The transdermal method is the best to quickly raise body’s magnesium levels and bring relief from pain anywhere in the body, but especially if in the lower leg area, as is often the case with PN.
- An Epsom Salt bath provides both magnesium and sulfur to the body. Dissolve 2 Cups Epsom salts (magnesium sulfate crystals) in a tub of warm (not hot) water. Soak whole body for 15-20 minutes. Do this therapy 3 times a week – Very relaxing!
Transdermal Magnesium Chloride
Vitamin D
#1 in the arsenal against inflammation
Vitamin D is neuroprotective
- Reduces neuronal loss when used alone in traumatic brain injury studies and further studies have shown that adding vitamin D to the Progesterone protocol to rebuild nerves, increases the benefits of Progesterone (See step 3 below). Vitamin D deficiency increases levels of inflammatory cytokines and proteins, which increase substantially when injured.
Best obtained from skin exposure to the sun’s rays
- Need 5000 – 10000 IU / day to battle neuropathic inflammation. The next best Vitamin D source is to use a full spectrum tanning bed, and the third choice is to take a vitamin D3 supplement.
“Anti-inflammatory/ Omega-6 GLA fatty acids
The body’s inflammatory response is controlled by the sufficient presence of anti-inflammatory Omega-3 and Omega-6 GLA fatty acids
- Balance today’s typical over-consumption of the inflammatory omega-6 fatty acids (E.g. in corn/soy/canola oils used in cooking /processed foods) – the best way to restore balance is to supplement with wild salmon oil or krill oil and flax seed for omega-3 and evening primrose or borage oil for omega-6 GLA
Castor Oil
Castor oil – Palm of Christ is used either alone or with added essential oils to relieve neural pain
- Some good warming E.O.’s: Oil of Oregano, Cinnamon Oil, Black Pepper Oil, and Ginger Oil, and also Cayenne
Curcumin for autoimmune PN
Potential neuroprotective properties of curcumin (found in turmeric spice)
- Curcumin, confirmed as potent inflammatory agent, and believed to interrupt immune system attack on myelin sheath. Nashville researchers believe curcumin may interrupt the production of IL-12, a protein that plays a key role in signaling immune cells to launch their assault on the myelin sheath.
- Mice with EAE (experimental autoimmune encephalomyelitis – an immune condition used as a model for MS, since it results in myelin erosion) recover movement after curcumin injections. In a 30-day study injecting mice with curcumin doses 3 times/week at doses roughly equivalent to the amount eaten in a typical Indian diet (E.g. in curry); In Asian countries, where spicy foods, including yellow compounds like curcumin are eaten quite regularly, reports of M.S. are rare; Annual Experimental Biology, 2002
Quit Smoking
Does this really need saying? OK fine – here’s just one reason.
- Smoking constricts the blood vessels that supply nutrients to the peripheral nerves and can worsen neuropathic symptoms.
Mainstream medicine symptomatic treatment for PN to control inflammation
Cymbalta
Cymbalta is a selective serotonin and norepinephrine reuptake inhibitor (SSNRI), FDA approved for PN
- An SSNRI prevents the reuptake of SEROTONIN and NOREPINEPHRINE by nerve endings, leaving these central nervous system (CNS) neurotransmitters active in the synaptic gap between neurons. In neuropathic pain, the nervous system itself is the source of pain. One of the things that the nervous system does is to filter out information being sent to it, so that only important information is sent on to the brain. One way that this happens is by having more of the neurotransmitters such as serotonin and norepinephrine present in the spinal cord and brainstem.
- Relief may not last more than a couple months and has some serious withdrawal problems – in some cases, Cymbalta works well for diabetes peripheral neuropathy for a couple of months but then, after realizing it doesn’t work anymore, it can take up to 3 months to completely wean off it, otherwise withdrawal symptoms can be severe. One site lists a possible 85 Cymbalta withdrawal symptoms. Some minor/irritating, such as canker sours, but others disruptive to daily life such as a buzzing in one’s brain.
Opiates
- Opiate-containing drugs can lead to dependence, constipation (opiates reduce intestinal motility) or sedation – E.g. codeine, oxycodone
- In many cases, peripheral neuropathy symptoms improve with time – especially if the condition is caused by an underlying condition that can be treated. A number of medications often are used to reduce the painful symptoms of peripheral neuropathy.
Pfizer’s Lyrica
FDA approved pill to treat nerve pain associated with diabetic neuropathy (and shingles) – it is the successor to Pfizer’s Neurontin, now also available as a generic. http://www.nytimes.com/2005/01/01/business/01pfizer.html?oref=login
- Lyrica appears to have some positive effects related to anxiety.
- Peripheral neuropathy may be associated with a deficiency of the neurotransmitter GABA – a possible reason for why Lyrica is effective against neuropathy pain. Dr. Braverman -“The Edge Effect“.

(2) Remove the source of damage to peripheral nerves
You need to address the source of your problem
- Diabetic neuropathy – you need to control blood glucose, which is causing high levels of oxidative stress throughout the body.
- Peripheral neuropathies, optic neuropathies, and pernicious anemia – can be due to a Vitamin B12 deficiency and/or folic acid deficiency.
- Neuropathy caused by exposure to toxic metals – E.g. lead, mercury, in medications. Focus on removing offending substances from the body.
- Neuropathy caused by bacterial infection – the only way to get rid of organisms in nerve sheath is using electromedicine.
- Neuropathies caused by an autoimmune disorder – E.g. rheumatoid arthritis, lupus, or Guillain-Barre – Treatment is aimed at the underlying inflammatory condition.
- Neuropathies caused by nerve pressure – E.g. carpal tunnel syndrome, trapped nerve. Focus on relieving the source of the pressure. Strategies include ergonomic changes to alter any repetitive motions or positions (such as at a keyboard) that caused the neuropathy, rebuilding cartilage, removing infection or toxins causing joint inflammation. Anti-inflammatory “tools” can be applied to area of spine with trapped nerve. (see above diagram) E.g. The SOTA magnetic pulser
Use electromedicine to kill bacteria inside myelin sheath
***HIGH PRIORITY***If mercury or other heavy metals could be present, then you should first do a treatment to remove them |
If you first apply electromedicine using a frequency of <10Hz to remove bacteria from the myelin sheath and mercury is present, these low frequencies can cause cells to become more permeable and mercury vapor can penetrate the brain. This could make the problem much worse; it is better to assume mercury is the problem and do a program to remove toxic metals first – if you are wrong, there is no harm done, only benefit. Suspect mercury poisoning if you have:
Treatment requires that toxic metals which can penetrate the blood brain barrier are removed from the body.The following link gives information on “tools” you can use to remove mercury and other toxic metals from your body. You must do your research on these, because some of the stronger methods of chelation can be dangerous if not done properly; helpful book on chelation: “My Recovery Protocol” by Ken Presner. Have dental amalgam removed by a QUALIFIED dentist – if this process is not done safely, it could kill you! Go to a “biological” or “holistic” dentist (NOT a regular dentist) – they are trained to do two things:
|
Electromedicine is the only way to kill bacteria, which are not in the blood stream – there are several choices of electrical units you can use for a systemic DAILY treatment to kill microbes (all are sold as research units, legally they cannot mention health benefits)
Here are a couple of choices of electromedicine devices:
(1) Beck Protocol Units – these are very affordable units that work very effectively to remove ALL microbes from the body that are not inside cells. One drawback is that the low output frequency (~4Hz) of these devices causes cell membranes to become very permeable, allowing many substances (E.g. mercury) to be absorbed into cell (technically called “transfection”, Beck called it “electroporation”). This means that the treatment would also increase the effect of any drugs you are taking, and as such, you cannot be taking any drugs concurrent with treatment. The transfection effect is less when using a device operating at a frequency of at least 10Hz (40 Hz is better if taking strong drugs), such as the “HIGH RF FREQUENCY GENERATOR” . However, using the 4Hz Beck Protocol unit, it may be possible to take some herbs or mild drugs, provided they are taken 2 hours before or 1 hour after daily electromedicine treatment session, to allow time for these substances to exit the body before the next day’s treatment session.
(2) “HIGH RF FREQUENCY GENERATOR”
- Versatile/powerful unit – “sweeps” through many frequencies in succession to target certain microbes. It runs frequencies up to 20 MHz (most other generators top out at < 40,000 Hz). Its 2.4 MHz ‘carrier wave carries lower frequencies far into the body. The “HIGH RF FREQUENCY GENERATOR” offers a selection of wave patterns, and several other features to set it apart; the major drawback to this generator is its price (~$2300-$4600 depending on options)
- Use programs for MS, Lyme Disease or any programs involving treponemes, spirochetes or mycoplasma (bacteria lacking cell walls)
Avoid / remove other harmful substances
Cleanse liver
Toxins may be responsible for PN and a poorly functioning liver will not be able to remove them from the body. A coffee enema is one of the best ways to stimulate the liver
Overnight liver/gallbladder flush (I won’t lie – this is not fun!)
Apply some natural detox therapies. E.g. Epsom salts, sea salt, seaweed powder, apple cider vinegar, and baking soda.
Foods to avoid
Avoid highly oxidized, damaged / processed fats (usually omega-6 fats) – E.g. trans fats found in most all processed / deep fried foods, typical grocery store oils (E.g. soy, canola, and corn oil), margarine, most peanut butter; Toxic Fats distort cellular functions throughout the body, including the brain.
Eliminate/minimize sugar, (particularly fructose, and minimize / eliminate other refined carbs) to control blood sugar
- Excess fructose and/or glucose promotes the production of significant damage / inflammation – causing AGES (Advanced Glycation End-products), which are involved in many degenerative diseases. Glycations to simple sugars, such as glucose and fructose, inactivates the enzyme glutathione reductase, responsible for maintaining the body’s major cell-protecting antioxidant enzyme Glutathione (GSH).
- Peripheral nerves and organs / tissue NOT dependent on INSULIN for their absorption of glucose are more susceptible to damage from periods of hyperglycemia than other organs/tissue – i.e. peripheral nerves, kidneys, blood vessels and lenses of the eye.
Cut out processed foods and sweetened beverages. This will go a long way to keeping fructose intake to a healthy level of < 25 grams / day.
Avoid refined carbs. The body quickly turns them into glucose; even whole grains convert to sugar, just a little slower. Tip: Eat sprouted grain bread and try and minimize even the whole grain carbohydrates in your diet
Too Much Sugar and Other refined carbohydrates
Avoid MSG – which has been linked to neuronal pathway damage
MSG – and other forms of Neurotoxic Free Glutamic Acid
Avoid aspartame, commercial fruit juices, bottled / canned fruits and vegetables – Aspartame (NutraSweet®, Equal®, etc.), typically found in sugar-free soda and foods, quickly metabolizes to methanol a potent neurotoxin. (Fresh fruit and veggies also contain methanol, but bound to pectin, and your body does not have the enzymes to break down this form. Unfortunately, the methanol in bottled / canned fruit or vegetables or their juice tends to dissociate from the pectin into free methanol, which you do absorb, and which is then converted into formaldehyde (yes, the same chemical they use to embalm dead bodies). Interestingly, ethanol (alcohol) is the antidote to methanol and could explain why moderate (one-a-day) “drinkers” often live longer than those who don’t drink! Epidemiologic studies show moderate consumption of alcohol is associated with a reduced risk of myocardial infarction, dementia, lupus, and other diseases of civilization.
Check your iron levels
Excess iron can cause damage – to the endothelium, the inner lining of blood vessels as well as create massive amounts of free radicals. It can also damage your DNA. Therefore, if you have PN it is very important to check your blood for iron overload, through a simple blood test called a serum ferritin test. The healthy range of serum ferritin is 20-80 ng/ml (ideally 40-60 ng/ml) ng/ml. Ferritin levels can even exceed 1,000, but anything over 80 is likely a problem. Donate your blood 1-3 times per year, even up to as many as once/month as tolerated, until your ferritin levels have been sufficiently lowered. Menstruating women would be unlikely to have excess iron, because they lose iron each month in blood lost during menstruation.
(3) Support nerves and aid peripheral nerve regeneration
Malabsorption Problems / Lack of nutrients or good intestinal bacteria
Malabsorption would obviously lead to nutritional deficiencies – Malabsorption may occur from a wide variety of causes:
- One common cause of malabsorption is a lack of beneficial intestinal bacteria needed to digest food. This can be corrected by taking a quality probiotic supplement with at least 50 billion CFU and a variety of good bacterial strains for a couple of months, whilst incorporating dietary probiotics (e.g. quality yogurt) and prebiotics (food for the good bacteria, such as bananas, garlic, onions, legumes, raw honey) into your ongoing daily regimen.
Eat lots of organic fruit & vegetables, organic eggs from pastured hens, and eat organic meats from grass-fed animals / birds – a raw egg smoothie (E,g, with fruit, yogurt and a banana) is an amazing pick-me-up for those who are ailing! Davidson’s™ eggs have been sterilized to ensure eggs are infection-free.
B vitamins
B vitamins are required for healthy nerve function. They may help those who develop peripheral neuropathy, especially when unassociated with a particular disease, such as diabetes. Generally, the B-vitamins help convert carbohydrates into energy. B6, B12 and Folate / folic acid (B9) in body) are cofactors for the methyl donor molecule SAMe. Regenerates nerves and promotes remyelination of nerve fibers. Since vitamins B6, B12 and folate are cofactors for SAMe, their deficiency may cause neurological and psychiatric disturbances, including depression, dementia, myelopathy and peripheral neuropathy, and folate deficiency has, in fact, been linked to PN. Sadun AA. Metabolic optic neuropathies. Semin Ophthalmol. 2002 Mar;17(1):29-32.
SAMe – And Other Methyl Donor Molecules
FOLIC ACID (B9)
Folic acid Dosage – the amount found effective in peripheral neuropathy is 10 mg – 2 to 3 times/day. Parry, T.E., Folate Deficient Neuropathy. ACTA Hematologica, 1990;84:108.
THIAMINE (B1)
Symptoms of B1 deficiency – include:
- Loss of appetite
- “Pins and needles” sensations
- Feeling of numbness, especially in the legs
- Muscle tenderness, particularly in the calf muscles
B1 as Benfotiamine is a naturally occurring, more bio-available form of B1 than conventional thiamine supplements
- Benfotiamine’s superior ability to penetrate cell membranes increases its bioavailability over conventional thiamine hydrochloride – its unique molecular open-ring structure enabling it to pass directly through cell membranes into the cell; Study in International Journal of Clinical Pharmacology Therapy found that the bioavailability of benfotiamine is 3.6 X greater than thiamine hydrochloride.
- Benfotiamine results in the sustained increase of Thiamine Pyrophosphate (TPP) – can produce beneficial effects on general nerve health, neuropathy, retinopathy, nephropathy, polyneuropathy, peripheral neuropathy, and coronary health for both diabetics and non-diabetics; German study found that benfotiamine can relieve neuropathy pain within 3 weeks.
- Benfotiamine contains sulfur
- Daily Dosage of Benfotiamine – 100 – 600mg w/food
Food sources of B1 – excellent B1 foods include Asparagus, Crimini Mushrooms, Spinach, Tuna, Brussels Sprouts, Flax seeds, Green Peas. Good sources are romaine Lettuce, mustard greens, summer squash, green beans, sunflower seeds, cabbage, tomatoes, turnip greens, broccoli, kale, cauliflower, black beans, oranges, bell peppers, swiss chard, navy beans, collard greens, dried peas, carrots, pineapple, lentils, garlic, lima beans, sesame seeds, pinto beans, grapes, cantaloupe, kidney beans
PYRIDOXINE (B6)
Daily Dosage of B6 – 2-8 mg Pyridixine HCl. Do not take more than 200 mg of B6 – as higher daily doses can actually cause symptoms of neuropathy.
COBALAMIN (B12)
Vitamin B12 protects the sheathing surrounding nerve cells and may promote regeneration and growth of nerve cells – a study in the Journal of Neurological Science postulated that methylcobalamine could increase protein synthesis and help regenerate nerves. Scientists state that ultra-high doses of methylcobalamine have been proven in clinical studies to produce nerve regeneration. Conversely, a B12 deficiency may result in nerve damage.
- The liver can store 3 – 5 years’ supply of Vitamin B12
- Food sources of B12: red meat, poultry, eggs, dairy products, fish
- Daily dose – 2000 mcg Methycobalamine (sublingual tablets) twice daily; typical doses range from 1000 – 5000 mcg; Methylcobalamine is more bioavailable than commonly supplemented cyanocobalamine;
Omega-3 – ***HIGH PRIORITY ***
The myelin sheath is primarily composed of fatty acids
- Optimize your essential fat intake – ensure a good supply of both animal and plant-based anti-inflammatory Omega-3 and omega-6 GLA fats for myelin sheath integrity (important for controlling extent of inflammatory reaction)
- The powerful “Omega-3 Fix” – incorporates sunbathing, flaxseed oil, flax seed with its fiber and lignans and a quality marine oil to supply a sufficiency of much needed, often deficient omega-3 fatty acids
Progesterone
Progesterone has been shown in animal studies to promote the formation of new myelin sheaths. Human Reproduction, 2000
- Progesterone promotes regeneration and myelination of axons (myelin forms around neural axons, allowing nerve impulses to travel faster); influences growth, differentiation and increases expression of myelin-specific proteins in oligodendrocytes, and potentiates the formation of new myelin sheaths by Schwann cells in vivo; antioxidant effect in injured nervous system; multiple effects on glial (Neuron support) cells;
- Progesterone-induced “blocking factor” directly blocks T-cell activation – reduces the expression of pro-inflammatory genes and their protein products.
- Progesterone is an essential building block for the stress hormone CORTISOL. Under stress, most of the progesterone produced is converted into the corticosteroid hormones to deal with the emotional stress or fight or flight situations.
- Adrenal exhaustion from aging / poor nutrition reduces adrenal progesterone production. Also reduces anti-inflammatory CORTISONE.
PROGESTERONE – “Precursor to Androgens, Estrogens and Corticoids”
Sulfur
- Component of B1 (thiamine). Important for nerve function.
- Component of antioxidants (E.g. glutathione, N-acetylcysteine (NAC), alpha-lipoic acid (ALA))
- Vitamin C is dependent on sulfur for absorption. For protection against potentially nerve-damaging oxidation reactions;
- Component of enzymes. E.g. Coenzyme-A;
- Bonds (S-S) connect proteins in connective tissue and are the basis for its flexibility. Important in neuropathy affected by connective tissue inflammation or degeneration;
- Has a role in detoxification – as a heavy metal detoxifier and especially in liver detoxification; free metal ions or other toxins may be the root cause of oxidative damage to nerves in PN.
L-Arginine
L-Arginine has potent neuroprotective properties. May be a therapeutic tool in ALS and neuropathy. Lee et al, 2009
NIR class 4 laser therapy
NIR Class 4 laser therapy is an effective healing frequency therapy in the infrared range (~700-1000 nanometers) obtainable at reasonable cost at clinics throughout the world, incl. the U.S. Not only stops the pain, but also affects a cure
- Reduces pain
- Reduces inflammation
- Enhances tissue healing
Lion’s mane mushroom
(saw this, might be worth researching)
Nerve regeneration using lion’s mane mushroom (Hericium erinaceus) – contains molecules known as hericenones and erinacines, two compounds suspected to stimulate nerve growth factor (NGF).
Other nutrients needed to maintain myelin sheath integrity
- Uric acid;
- Vitamin D
- Essential fatty acids;
References
Annual Experimental Biology (2002) Conference New Orleans, LA April 23, 2002
Human Reproduction 2000 Jun;15 Suppl 1:1-13, J Steroid Biochem Mol Biol 1999 Apr-Jun;69:97-107, Mult Scler 1997 Apr;3:105-12 PubMed
Kingery WS. (1997) A critical review of controlled clinical trials for peripheral neuropathic pain and complex regional pain syndromes. Pain ;73:123-39.
Kahler W, Kuklinski B, Ruhlmann C, et al. (1993) Diabetes mellitus-a free radical-associated disease. Results of adjuvant antioxidant supplementation [in German; English abstract]. Z GesamteInnMed.48:223-232.
Lee J, Ryu H, Kowall NW. Motor neuronal protection by L-arginine prolongs survival of mutant SOD1 (G93A) ALS mice. Biochem Biophys Res Commun. 2009 Jul 10;384(4):524-9. PubMed
Love A, Cotter MA, et al. (1996 Aug) Effects of the sulphydryl donor N-acetyl-L-cysteine on nerve conduction, perfusion, maturation and regeneration following freeze damage in diabetic rats. Eur J Clin Invest. 26(8):698-706. PubMed
Packer L, Witt EH, Tritschler HJ. (1995) Alpha-lipoic acid as a biological antioxidant. Free Radic Biol Med. 19:227-250.
Ruhnau KJ, Meissnert HP, Finn JR, et al. (1999) Effects of 3-week oral treatment with the antioxidant thioctic acid (alpha-lipoic acid) in symptomatic diabetic polyneuropathy. Diabet Med. 16:1040-1043.
Sagara M, Satoh J, Wada R, Yagihashi S, Takahashi K, Fukuzawa M, Muto G, Muto Y, Toyota T. (1996 Mar) Inhibition of development of peripheral neuropathy in streptozotocin-induced diabetic rats with N-acetylcysteine. Diabetologia. 39(3):263-9. PubMed
Ziegler D, Hanefeld M, Ruhnau KJ, et al. (1995) Treatment of symptomatic diabetic peripheral neuropathy with the antioxidant alpha-lipoic acid. A 3-week multicentre randomized controlled trial (ALADIN Study). Diabetologia. 38:1425-1433.
Ziegler D, Gries FA. (1997) Alpha-lipoic acid in the treatment of diabetic peripheral and cardiac autonomic neuropathy. Diabetes. 46(suppl 2):S62-S66.