Atherosclerosis process - How and why does atherosclerotic plaque build up in arteries?
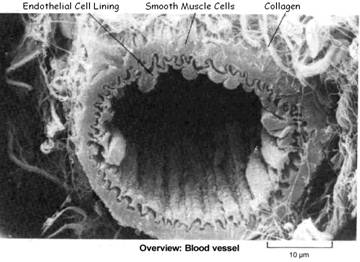
Endothelium - a single layer of Endothelial Cells (ECs) lines the inside of the blood vessel wall
To avoid a blood vessel rupturing consequential to various injurious mechanisms to a weakened endothelial artery lining:
- The damage irritates /inflames the endothelium causing an inflammatory immune response for the purpose of healing or controlling the damage.
- The arterial wall ECs initiate life-saving action to “beef up” the damaged wall by depositing an artery-thickening layer of plaque.
(1) The ACUTE PHASE inflammatory response is a necessary and appropriate response to injury or infection
Without inflammation infections would go unchecked and wounds would never heal
The damaged site becomes red, swollen and warm as healing mechanisms are initiated. The acute phase response occurs within minutes to hours, but if the infection or injury continues and/or the problem is not resolved within a few days, it becomes a chronic inflammatory response.
Acute phase protein (APP) molecules (cytokines and acute phase reactants) orchestrate the responsive action
- Released in response to alarm-signaling cytokines (particularly IL-6) – by most cells (in particular in the arteries, by various immune system cells, E.g. T-cells, macrophages, platelets, and ECs) during infection or injury;
- Acute Phase Reactants (APRs, a type of APP) are produced (mostly in the liver) and released into the plasma –modulate blood clotting, vessel dilation/ contraction, fibrosis (repair fiber/scarring), cell proliferation, immune cell action, cholesterol deposit/removal, and more.
Acute Inflammation Response
- Vessels dilate for 15 minutes to several hours and become more permeable. Enabling WBCs and fluids to leave the vessels (manifests as swelling);
- Phagocytic WBCs adhere to vessel wall. Cytokines increase number of EC adhesion molecules, which then adhere phagocytic WBCs (usually neutrophils) to the vessel wall, which engulf and destroy microbes and debris particles. (In viral infection, lymphocytes rather than neutrophils usually predominate. In certain parasitic infections, eosinophils predominate);
- Injurious agents are destroyed or walled off and debris is cleared. By activated specialized blood and connective tissue cells, so that tissue repair can take place;
- Blood clot is formed. To prevent blood loss and provide a barrier to microorganisms;
- Fibrous connective tissue is brought in to repair the damage;
- When healing is complete the blood clot is removed.
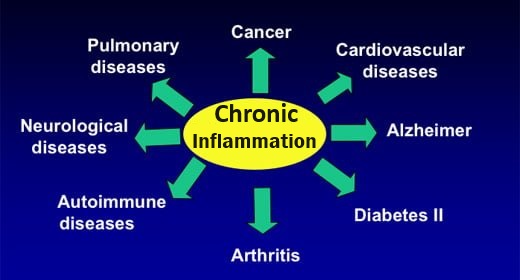
(2) CHRONIC inflammatory response leads to endothelial dysfunction and eventually the development of atherosclerotic plaque
Inappropriate, prolonged inflammatory response to ongoing endothelial injury leads to:
- Endothelial dysfunction as a consequence of sustained vessel constriction / high blood pressure (mainly as a consequence of insufficient available, endothelium-relaxing nitric oxide)
- Further increases in coagulation, vessel adhesion molecules, and immune system white blood cell activity.
- The process culminates in the development of atherosclerotic plaque.
Chronic inflammation in the arterial endothelium involves:
- Vessel constriction. Due to failure of endothelium-dependent relaxation mechanism;
- Macrophages and Lymphocytes. Accumulation of immune system macrophages (engulf and destroy bacteria / debris/cholesterol) and lymphocytes (T-cells, B-cells, NK cells);
- Tissue Damage. Generation of damaging ROS in ECs, smooth muscle cells (SMCs) and adventitia, responsible for tissue destruction, as seen in CVD (and auto immune and neurodegenerative disease);
- Life-saving Atherosclerotic Plaque. Chronic endothelial injury requires a more substantial, artery-thickening, “repair patch”as a life-saving measure to prevent arterial rupture (artery is under high pressure), consisting of oxidized cholesterol, fat, smooth muscle cells, macrophages, T-cells, fibrous tissue and calcium deposits.
This stronger repair process involves:
- Vascular smooth muscle cell proliferation
- Development of fibrosis – excess fibrous connective tissue, mainly collagen and elastin.
- Accumulation of cholesterol – which becomes oxidized and develops into foam cells and fatty streaks (via immune system monocytes/macrophages).
(3) Eventually the artery is partially or fully occluded
- By the physical obstruction of atherosclerotic plaque itself
- Or more often by blood clots (thrombi) formed by plaque rupture, which results in reduction of blood flow (ischemia)
- Or by a piece of plaque breaking off and traveling to and blocking smaller arteries, such as the carotid artery
Possibly resulting in:
- Damage to heart muscle (by blocking a coronary artery) →→→HEART ATTACK
- Damage to brain (by blocking a carotid artery) →→→ STROKE / CAROTID ARTERY DISEASE (>95% of cerebrovascular disease)
- Damage to nerves and tissues in legs and feet (by blocking an iliac artery) →→→ PERIPHERAL ARTERY DISEASE (PAD)