Breast cancer

Overview of this all too prolific cancer
Most common types of breast cancer
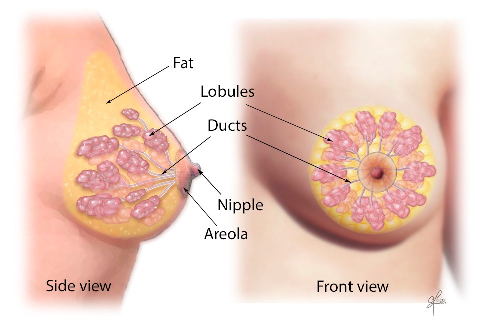
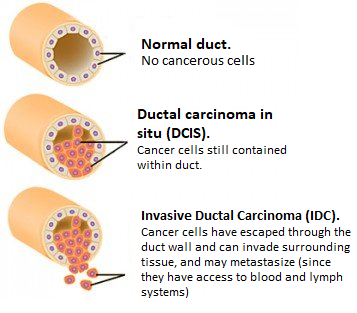
Ductal carcinoma in situ (DCIS) (majority of breast cancers). Originates in the cells lining the milk
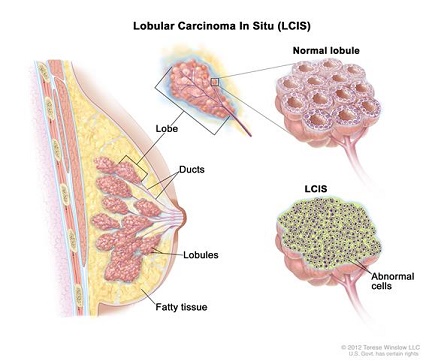
Lobular carcinoma in situ (LCIS) Originates in the lobules.
Less common, types of breast cancer include: Medullary, Mucinous, Tubular, Metaplastic, Papillary breast cancer, Inflammatory breast cancer (a faster-growing type, ~1 – 5% of all breast cancers), Paget ‘s disease (cancer begins in the nipple ducts).
Breast cancer metastases
Breast tumour cells can metastasize (i.e. spread) to the axillary lymph nodes and to other organs, most often the bones, brain, liver and lungs. Breast cancer cells can break away from the primary tumor and enter the bloodstream or lymphatic system, where blood or lymph fluids can transport the cells around the body. The cells can then settle and form new tumors in places far from the original tumor. Commonly, doctors diagnose metastatic breast cancer after previously received treatment for an earlier stage (non-metastatic) breast cancer. When invasive surgery cuts into breast tissue to remove a tumor, there is an obvious risk that cancer cells will enter the bloodstream and metastasize.
A 2018 Finnish / Swedish study examining the routes of metastases in breast cancer (by studying cancer cell DNA) found that metastases do NOT spread from axillary lymph nodes. “. . . metastases in the axillary lymph nodes do not seem to spread further to other organs, so even if these metastases can show how aggressive the cancer is, it is not they that cause the spread,” says Johan Hartman, Associate Professor at Karolinska Institutet’s Department of Oncology-Pathology, one of the researchers who led the study. The study also found that in certain cases an early explosion of cancer cells from the breast tumour simultaneously gives rise to metastases in several different organs. The researchers also showed that different regions of the breast tumours caused metastases in specific organs in the body. Ullah et al, 2018
Incidence and death rates
On a positive note: 80% of identified breast lumps are NON-cancerous.
Globally. Breast cancer is the secondmost common cancer killer of women – only lung cancer is more deadly. Worldwide, in 2022, 2.3 million women were diagnosed with breast cancer, which caused 670,000 deaths. Countries with a high development index (hdi) have up to twice as many breast cancer diagnoses (1 in 12 in their lifetime, and 1 in 71 die of breast cancer) compared to women in a low HDI country (1 in 27 diagnosed, and up to 1 in 48 women die). WHO
In the U.S.
- American Cancer Society 2025 data estimates 316,950 new breast cancer cases for women (2,800 for men), and 42,170 women will die from this prolific disease (also 510 men).
- The rate of new cases of female breast cancer was 130.8 per 100,000 women per year. The death rate was 19.2 per 100,000 women per year. These rates are age-adjusted and based on 2018 – 2022 cases and 2019 – 2023 deaths.
- Lifetime Risk of Developing Cancer: Approximately 13% (one out of 8) women will be diagnosed with female breast cancer at some point during their lifetime, based on 2018 – 2021 data (excluding 2020 due to COVID).
- 80-85% of women diagnosed with breast cancer have no family history of breast cancer. PubMed In a large Chinese study, family history of breast cancer mainly influenced patient age, tumor stage, and grade at diagnosis. Correlation between family history and characteristics of breast cancer.
- Breast cancer is the leading cause of death for Non-Hispanic black women and Hispanic women.
- 15% of all breast cancers occur in women under age 45. Generally, they have more aggressive cancers with lower recovery rates.
- 89% of women diagnosed with breast cancer have no family history of this disease in mother, daughter or sister. Collaborative Group on Hormonal Factors in Breast Cancer. Familial breast cancer, 2001.
- <10% of breast cancer cases are thought to stem from inherited gene mutations. E.g. BRCA1 and BRCA2, which individually substantially increase risk. However, cellular changes by genes are not inherited, they occur in response to the body’s terrain, such as the presence of environmental carcinogens, or excessive exposure to circulation hormones..
- About 90% of women diagnosed with breast cancer have a type of cancer called estrogen receptor postive (ER+). which means that the cancerous tissue contains receptors for the sex hormones Aout half of the ER+ cancer cases also contain progesterone receptors (abbreviated ER / PR+). Hormone-receptor negative (HR-) lacks receptors for estrogen or progesterone, is more likely to occur in premenopausal women, and is more aggressive and harder to treat than HR+ cancer.
- Triple negative breast cancer (TNBC). Is not only ER- and PR- , it is also negative for human growth factor receptor 2 (HER2), which aids cancer cell growth.
- Men are not immune from getting breast cancer. Although <1% of cases. Men who work around gasoline and combustion products have a significantly higher risk of developing breast cancer. American Journal of Industrial Medicine 2000;37:349-352 –

Are mammograms beneficial?
- More than half of breast cancers are found by other than mammograms. The 2003 National Health Interview Survey (NHIS), a nationally representative self-report health survey, included 361 women survivors diagnosed with breast cancer between 1980 and 2003. Responses to the question, “How was your breast cancer found?” determined 57% of breast cancer was found by self-examination, by accident or by a a physician during a breast examination. 43% were detected by mammography. PubMed.
- A number of studies have found that routinely screening healthy middle-aged women for breast cancer does not lower death rate, additionally finding that aggressively screening the general population can cause harm. An extensive Canadian study in the British Medical Journal, involving 90,000 women followed over 25 years in a randomized trial, found that efforts to find breast cancers before they could be felt as a lump in the breast, using screening mammography, did not lead to lower death rates for average-risk women in their 40s and 50s. At the same time, around one in five of the cancers that were found through screening would not have required treatment were it not for the mammogram: resulting in overdiagnosis and overtreatment as these women underwent surgery, radiation, and chemotherapy to treat non-life threatening cancers.
- Furthermore, research confirms that cumulative radiation from routine mammograms may actually cause breast cancer.

What are the causes / risk factors of breast cancer?
Lifestyle / environmental / conditional factors
Research at the American Institute of Cancer Research estimated that about 40% of U.S. all cancer cases and about half of the cancer deaths could be prevented by making better lifestyle choices. Modifiable risk factors include cigarette smoking (leading contributor to cancer deaths 32.2% in men, 24.4% in women), body weight, infection, alcohol consumption, physical inactivity, diet, stress and uv radiation. Proportion and number of cancer cases and deaths attributable to potentially modifiable risk factors in the United States, 2019, published 2024 in American Cancer Society journal
Paleoanthropological research shows that cancer was virtually nonexistent in humans before poor diet and pollution appeared. Cancer: an old disease, a new disease or something in between?
Iron and aluminum toxicity in breast cancer
Genes do not have the last word. Breast cancer risk increases <10% with a family history of the disease. Mutations of the BRCA1 and BRCA2 genes are said to increase breast cancer risk substantially, however, it is the expression of your genes that dictates the risk, and not simply their existence. Gene expression can be controlled (by whether they are turned on or not) via lifestyle and dietary choices.
Conditional factors that increase relative risk for breast cancer (BC) in women
| Relative Risk | Factors |
|---|---|
| > 4.0 | Female Age > 65 – although risk increases across all ages until 80. Inherited mutations for breast cancer (BRCA-1 or BRCA-2) 2 or more. 1st-degree relatives diagnosed with BC at an early age. Personal history of BC. High breast tissue density Biopsy confirmed atypical hyperplasia |
| 2.1 – 4.0 | One 1st-degree relative with BC. High dose radiation to chest. High bone density (post-menopausal) |
| 1.1 – 2.0 Factors affecting circulating hormones | Age >30 years at 1st full-term pregnancy. Menarche before age 12 years. Menopause > 55 years. No full-term pregnancies. Never breast-fed a child. Recent oral contraceptive use. Recent and long-term use of hormone replacement therapy. Postmenopausal obesity |
| 1.1 – 2.0 Other Factors | Personal history of endometrium, ovary or colon cancer. Alcohol consumption* Tall height. High socio-economic status. Jewish heritage |
* More than 2 alcoholic drinks/day. According to data published in the British Journal of Cancer in 2002, 4% of all breast cancers (~44,000 cases a year) in the United Kingdom are due to alcohol consumption. Could this be due to magnesium depletion in the body consequential to drinking alcohol? See: Magnesium against Cancer
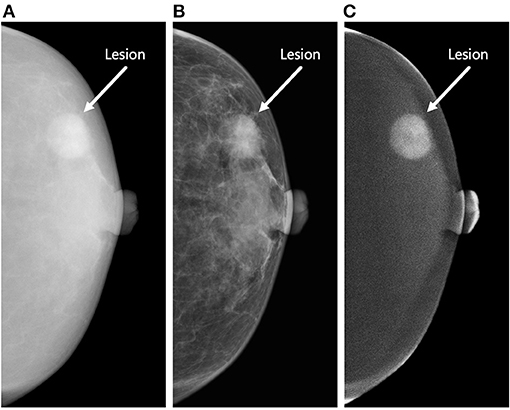
Almost half of women have dense breast tissue affecting ability to see abnormal tissue on mammogram
Tumors and calcifications show up white, as does dense breast tissue.
Dense breasts have relatively high amounts of glandular and connective tissue compared to fatty tissue. The diagram below shows increasing levels of glandular / connective tissue density, which can only be seen on mammograms and can not be felt via physical examination. Breasts are classified as dense if they fall into the (C) and (D) classifications:
- (A) Almost all fatty breast tissue (10% of women)
- (B) Scattered dense glandular / connective tissue (40% of women)
- (C) Hetererogeneously dense breast tissue with many areas of dense glandular / connective tissue (40% of women)
- (D) Extremely dense tissue (10% of women)
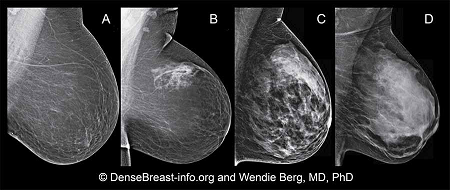
Although often inherited, other factors can influence breast density. Including increasing age, having children and using the estrogen-lowering drug Tamoxifen. Breast tissue density is also associated with having a low body mass and using postmenopausal hormone replacement therapy.
Having dense breast tissue does not increase death rate from breast cancer. Although having high breast tissue increases risk for breast cancer, research shows that a woman with dense breast tissue is no more likely to die from breast cancer than a woman with fatty breast tissue.
The estrogen hormone estradiol speeds up breast cancer in estrogen receptor-sensitive cancer types
Double blind, placebo controlled, randomized study used transdermal progesterone and estradiol on 40 premenopausal women undergoing breast surgery for the removal of a lump. The study examined results of two breast biopsies, one at the beginning of the study and another 13 days later. Estrogen and the progesterone did not show up in the serum, but showed up in the breast tissue at over 100% increased levels above placebo. Chang et al, 1995
Results of breast tissue cell proliferation from biopsies after 13 days transdermal progesterone or estradiol administration:
| Method of Measuring Cell Proliferation ▼ | Placebo | Progesterone | Estradiol |
|---|---|---|---|
| Mitosis per 1000 Cells | 0.51 | 0.17 | 0.83 |
| PCNA (proliferating cell nuclear antigen) – the most accurate method | 7.8 | 1.9 | 17.4 |
Study concluded that in normal breast tissue:
- Increased estradiol concentration increased cell proliferation
- Exposure to progesterone for 10-13 days reduced estradiol-induced proliferation
Based on PCNA numbers (PCNA presence in actively growing and dividing cells serves as a marker for such cells):
- Topical progesterone reduced ▼cell proliferation by 410%
- Topical estradiol increased ▲cell proliferation by 223%
progesterone levels naturally decrease with age. In women this decrease occurs about the age of 35 and men about ten years later. progesterone balances estrogen, such that an imbalance of estrogen over progesterone could be responsible for increased cell proliferation in estrogen-sensitive breast cancer.

What measures can I take to prevent breast cancer?
Vitamin D / Sunshine is the #1 cancer fighter
- Cheap and natural solution
- This steroid hormone has receptors in and influences almost all body cells. Once converted to its active form (Calcitriol) in the liver, kidneys and other tissues, your organs use it to repair damage and reduce cancer cells.
- Increases self-destruction of mutated cells. Prevents their replication; cancer cells usually begin as mutations.
- Shown to shrivel up cancer cells in days. Vitamin D and Cancer: JoEllen Welsh, State University of New York at Albany
- Reduces spread/reproduction of cancer cells.
- Causes cell differentiation. Cancer cells often lack differentiation, whereby a cell becomes more specialized by changes (mainly due to modifications in gene expression) in shape, size, membrane potential, metabolic activity and signal responsiveness.
- Reduces new blood vessel growth from existing ones. Angiogenesis is a step in the transition of dormant tumors becoming cancerous.
- Ideal level circulating CALCIDIOL (25(OH)D) is 65 – 90 ng/ml
- Synergistic with other cancer treatments
- Prevents many cancer deaths. One landmark study examining just breast and colorectal cancer deaths, determined that increasing vitamin D could prevent 600,000 deaths each year.
- Vitamin D is effective against at least 16 cancer types
- Found to work well as an adjuvant with Tamoxifen. Dr.Zheng et al, 2018
Emotional control
- Address stress. E.g. Using Meridian Tapping Technique (MTT) or SOTA Brain Tuner.
- Work on positive attitude
Iodine
Supplement with Iodine. Prevents cancer formation and spread, especially reproductive organ cancers.
Avoid excess Iron
Excess iron contributes to oxidant activity. Ferritin, the iron transport protein, tends to increase after menstruation ceases; should not be above 80; donating blood lowers ferritin level;
Iron and Aluminum toxicity in breast cancer
Don’t wear a bra
Do not have mammograms
They do not save lives!
Instead, do regular self-examinations of breasts or find a doctor who does thermography– this non-invasive method is based on heat detection, does not compress breast and does not use harmful radiation, which can actually cause breast cancer when accumulated over time.
Eat nutritional food
- Don’t eat processed / refined foods;
- Antioxidants. Especially vitamins A, C, E, and ubiquinol (active form of CoQ10); antioxidants control radical damage implicated in cancer; fight microbial imbalance;
- Omega – 3. E.g. as krill oil or wild salmon oil) shown to influence BRCA1 and BRCA2 genes against cancer;
- Eat broccoli or broccoli sprouts;
Regular moderate physical exercise
Take a daily 20-30 minute brisk walk
Reduce body’s estrogen levels
There are several tactics you can use to reduce estrogen in the body:
How to reduce body’s estrogen levels
For example:
- Maintain a healthy body weight. Estrogen hormone is produced in fat tissue, and may trigger breast cancer.
- I3C / DIM. Phytochemicals such as indole-3-carbinol (I3C) and sulforaphane are components of cruciferous vegetables which exhibit antitumorigenic activity associated with altered carcinogen metabolism and detoxification. Diindolylmethane (DIM) is a major metabolite of I3C formed in the gut and represents a new class of antiestrogens that inhibit breast cancer growth. It also encourages cells that are abnormally multiplying to stop reproducing and die.
Researchers have found that DIM and genistein (a major isoflavone in soy) reduce production of two proteins whose chemotactic attraction to each other is necessary for the spread of breast and ovarian cancers. When applying purified versions of DIM and genistein to motile cancer cells, the researchers could literally watch these cells come to a near halt. When either compound was applied, migration and invasion were substantially reduced. Both DIM and genistein are already being developed for use as a preventive and a chemotherapy treatment for breast cancer, although more extensive toxicological studies are necessary as at the time of writing (2007).
DIM – Estrogen – blocker with anti – cancer benefits
Miscellaneous
- Limit alcohol to one or two drinks a day
- Breast feeding exclusively for up to six months reduces breast cancer risk;
- Improve INSULIN receptor sensitivity. Exercise and control intake of refined carbs and sugar; iodine also helps improve receptor sensitivity.

How to treat breast cancer
+ (1) Cancer Treatment Core
Of special mention
Baking soda / Maple Syrup Protocol. Baking soda alkalizes cells. Researchers have found that this protocol inhibits malignant growth by increasing tumor pH, and also reduces formation of spontaneous metastases. The sudden pH increase kills the cancer cells. as the shock of alkalinity allows more oxygen into the cancer cells than they can tolerate. (OR If, like this author,you hold with the microbial theory of cancer, it causes cancer microbe inside cells to die or go into its hibernating form, such that cells revert to normal metabolism. Baking Soda / Maple Syrup against Cancer
Magnesium. Magnesium against Cancer Without sufficient magnesium, the body accumulates toxins and acid residues and degenerates rapidly. For any degenerative disease, especially cancer, transdermal or nebulized magnesium chloride is a “No-brainer” to quickly build up the body’s magnesium levels.
(2) Eliminate cancer cells
Treatment options: depend on the stage of cancer development and your choices are presented in the
Treatments of special note for breast cancer:
Blocking estrogen stops / slows estrogen-sensitive breast cancer
The American Cancer Society estimates that 2 out of 3 breast cancer cases are hormone-receptor positive. If breast cancer displays estrogen receptors, then reducing estrogen levels in the body, in addition to other treatments, is potentially beneficial (since estrogen stimulates cancer growth) (a receptor is a structure on the surface of a cell that selectively receives and binds substances). A Basic Review on Estrogen Receptor Signaling Pathways in Breast Cancer Laura P Stabile et al, 2002
Estrogen dominance is a prevailing problem in today’s world
It’s all about the receptors! A large international breast cancer research team (published in “Nature”), made the eye-opening discovery of how receptors that mediate activity of the female sex hormones (estrogen and progesterone) interact with DNA to control the growth of hormone-receptor positive breast cancers. Mohammed et al, 2015.
- Estrogen activates estrogen receptors, which are agents that turn on cancer-promoting genes in breast cancer.
- Progesterone activates progesterone receptors, which bind to and ‘reprogram’ estrogen receptors, transforming them into agents that turn on genes to slow down or reverse the cancer cell growth.
The researchers emphasize that their conclusions ONLY apply to natural, BIOIDENTICAL progesterone
Premarin + Provera combination shown to increase risk of breast cancer (also endometrial and ovarian cancers)
The Woman’s Health Initiative (WHI) study demonstrated that a combination of the synthetic estrogen and progesterone hormones Premarin™ (conjugated equine estrogens (CEEs, primary ingredients: sodium estrone sulfate and sodium equilin sulfate, which convert to ESTRADIOL, then estrone) and Provera (the progestin Medroxyprogesterone acetate (MPA)),produces a 26% increase in invasive breast cancer. Rossouw et al, 2002
The risk of breast cancer was significantly greater with HRT utilizing CEE’s with Provera) ™(containing the progestin MPA) than with HRT containing micronized progesterone. Fournier et al, 2005 or when utilizing a non-CEE estrogen combined with a progestin other than MPA de Lignières et al
Synthetic Sex Steroids – “Frankinstein Forms
The scientists in the above 2015 study published in “Nature” reiterate the findings of Drs. Zava and Lee in 2002:
Women with estrogen dominance, where progesterone levels are low relative to estrogen levels, are more likely to get breast cancer and have poorer treatment outcomes. Drs Zava and Lee and Virginia Hopkins, coauthors of What Your Doctor May Not Tell You About™ Breast Cancer, concluded that estrogen dominance causes estrogen receptors to activate genes such as BCL-2 that are known to promote the rapid growth of cancer cells.
When progesterone is raised to healthy levels relative to estrogen, it turns on genes that can prevent breast cancer from occurring and reduce the size of existing tumors. Dr. Lee and Dr. Zava cited research showing that progesterone receptors activate genes such as p53 that promote apoptosis (body’s method of destroying cancer cells before they develop into tumors).
Since dominance over progesterone is a common problem today BIOIDENTICAL PROGESTERONE supplementation in hormone-sensitive breast cancers could indeed increase survival rates.
DIM supplementation proven to be beneficial in reducing estrogenic activity in the body. DIM demonstrated anti-cancer mechanisms in lung cancer in mice and human studies. Morse MA et al, 1990; Ichite N et al, 2009
I3C / DIM – Estrogen Blocker with Anti-cancer benefits
MELATONIN has multiple anti-estrogen actions and decreases estradiol levels in the body in lung cancer.
- MELATONIN has been used both alone and in combination with most standard cancer treatments because it improves both survival and quality of life. Lynch E, 2005
- MELATONIN combined with aloe vera extract stabilizes the cancer growth and improves survival in advanced cancer patients. In a study including 50 patients (with advanced, untreatable neoplasms for whom no other standard treatment is offered) suffering from lung cancer, gastrointestinal tract tumors, breast cancer or brain glioblastoma. Patients were treated with melatonin (MLT) alone (20 mg/day orally when dark) or MLT plus aloe vera tincture (1 ml twice/day). Lissoni P et al., 1998
- A partial response (PR). Achieved in 2/24 patients treated with MLT plus aloe and in none of the patients treated with MLT alone.
- Stable disease (SD). Achieved in 12/24 and in 7/26 patients treated with MLT plus aloe or MLT alone, respectively.
- The 1-year survival rate. Significantly higher in patients treated with MLT plus aloe (9/24 vs. 4/26, p < 0.05).
- MELATONIN has multiple anti-estrogen actions and decreases body’s estradiol levels. Sanchez-Barcelo EJ, 2005; Rato AG et al, 1999
Vitamin K2. Vitamin K2 – For Klotting and Kalcium reduces estrogenic activity in body. Vitamin K2 (menaquinone) decreases the ratio of estradiol to less estrogenic estrone. Known for its blood coagulation effects, K2 also reduces estrogenic activity. Otsuka M et al, 2005
Estrogen levels lowered by maintaining healthy body weight. Body fat is a source of estrogen; therefore it is important to establish and maintain a healthy body weight. Siiteri PK, 1987
Cesium Chloride
There was an impressive 50% recovery of various cancers. i.e. cancer of unknown primary, breast, colon, prostate, pancreas, lung, liver, lymphoma, ewing sarcoma of the pelvis and adeno-cancer of the gallbladder, by utilizing cesium therapy. Sartori HE, Cesium therapy in cancer patients (1984). Pharmacol Biochem Behav. 21 Suppl 1:11-3 PubMed.
CESIUM CHLORIDE / DMSO PROTOCOL
Iodine
Iodine has several roles in both the prevention and treatment of cancer. Especially in thyroid cancer and the reproductive organ cancers.
Lorem ipsum dolor sit amet, consectetur adipiscing elit. Ut elit tellus, luctus nec ullamcorper mattis, pulvinar dapibus leo.

References
Chang KJ, Lee TTY , Linares-Cruz G, Fournier S, de Lignieres B (1995) Influences of percutaneous administration of estradiol on human breast epithelial cell cycle in vivo. Fertility and Sterility; 63; 7865-7891. Online link
Collaborative Group on Hormonal Factors in Breast Cancer. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet. 2001;358(9291):1389–1399. PubMed
Ikram Ullah, Govindasamy-Muralidharan Karthik, Amjad Alkodsi, Una Kjällquist, Gustav Stålhammar, John Lövrot, Nelson-Fuentes Martinez, Jens Lagergren, Sampsa Hautaniemi, Johan Hartman, Jonas Bergh (2018) Evolutionary history of metastatic breast cancer reveals minimal seeding from axillary lymph nodes. Journal of Clinical Investigation; DOI: 10.1172/JCI96149
Ullah I, Karthik GM, Alkodsi A, Kjällquist U, Stålhammar G, Lövrot J, Martinez NF, Lagergren J, Hautaniemi S, Hartman J, Bergh J. Evolutionary history of metastatic breast cancer reveals minimal seeding from axillary lymph nodes. J Clin Invest. 2018 Apr 2;128(4):1355-1370. doi: 10.1172/JCI96149. Epub 2018 Feb 26. PMID: 29480816; PMCID: PMC5873882. PubMed
Hormone-sensitive breast cancer studies
Mohammed, Hisham, et al (2015) Progesterone receptor modulates ER-a action in breast cancer. Nature ; 523; 313-317. Link.
Perks, Bea (17 Jul 2015) Progesterone receptor could slow breast cancer growth. Pharmaceutical Journal. Link.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J (2002 Jul 17) Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 288(3):321-33 PubMed
de Lignières B, de Vathaire F, Fournier S, Urbinelli R, Allaert F, Le MG, Kuttenn F. (2002 Dec) Combined hormone replacement therapy and risk of breast cancer in a French cohort study of 3175 women. Climacteric. 5(4):332-40. Researchgate
Fournier A, Berrino F, Riboli E, Avenel V, Clavel-Chapelon F. (2005 Apr 10) Breast cancer risk in relation to different types of hormone replacement therapy in the E3N-EPIC cohort. Int J Cancer. 114(3):448-54. PubMed
Laura P. Stabile, Autumn L. Gaither Davis, Christopher T. Gubish, Toni M. Hopkins, James D. Luketich, Neil Christie, Sydney Finkelstein and Jill M. Siegfried. Human Non-Small Cell Lung Tumors and Cells Derived from Normal Lung Express Both Estrogen Receptor α and β and Show Biological Responses to Estrogen. Cancer Res April 1 2002 (62) (7) 2141-2150; Link