Thyroid Hormones T3 / T4 - "Master Metabolism Hormones"
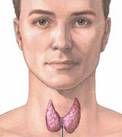
Triiodothyronine (T3) and thyroxine (T4) are produced by the thyroid gland
The thyroid gland (The body’s “thermostat”) is a butterfly-shaped gland wrapped around the windpipe. Behind and below the Adam’s apple.
The thyroid gland produces thyroid hormones Thyroxine (T4) and Triiodothyronine (T3) inside its thyroid follicles
- T4 – Storage form
- T3 – Metabolically active form
Active-form T3 has three primary functions:
- Enhance protein synthesis and growth
- Help oxygen get into cells – determines how quickly the body uses energy (the basal metabolic rate (BMR)). Increasing cellular oxygen consumption increases production of cellular ATP (cell’s energy currency)
- Control body’s sensitivity to other hormones
T3 influences every organ, tissue and function in the body:
| Heart rate | Body weight | Connective tissue integrity / Nerve and bone formation |
| Energy level, | Muscle strength | Rate food moves through GI tract |
| Menstrual regularity | Body temperature | Speech / mental state |
| Reproduction | Hair, skin, nails, teeth condition |
Thyroid Hormones T4 =>Active T3 Conversion
- All the thyroid hormone metabolic activity comes from T3 – T4 is the body’s storage form ready to be converted to its active T3 form (Except during pregnancy, when T4 is needed for the fetus to develop properly).
- Only ~20% of the body’s T3 comes from the synthesis of T3 within the thyroid – the rest of the T3 is derived when the deiodinase enzyme removes one iodine molecule from T4. (the “3” and “4” refer to the number of iodine atoms in each thyroid hormone molecule).
- Most T4 →T3 conversion (via deiodinase enzymes) takes place in the liver – but some also in muscles and other peripheral organs, including thyroid, kidneys, spleen and the brain’s hypothalamus. The immediate effects of T3 last for 1-2 days.
- Some people have a problem converting T4 to T3 not always indicated by lab tests.
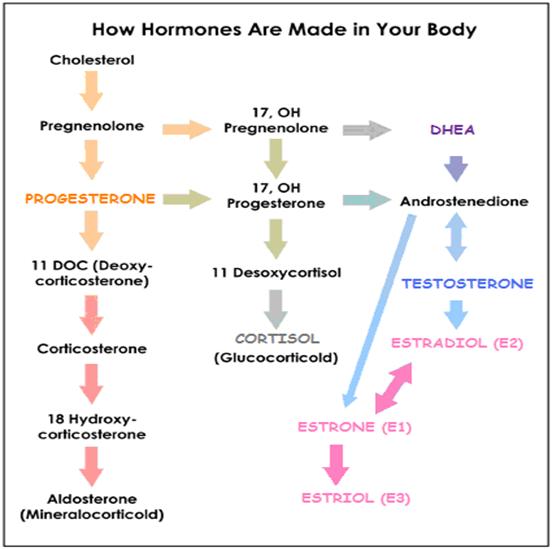
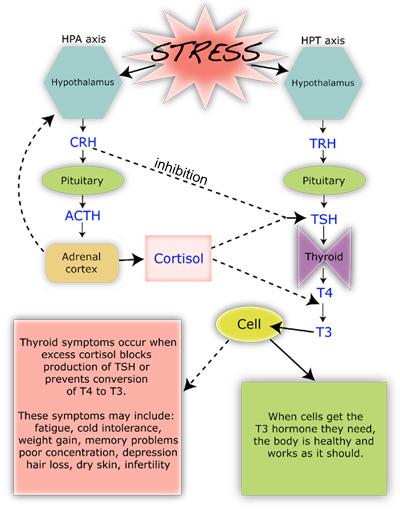
- Stress-activated hormones interfere with T4 to T3 conversion – stress hormones, such as CORTISOL and EPINEPHRINE (ADRENALINE) can divert the conversion of T4 hormones into inactive forms that do not activate metabolism.
Thyroid production support
The thyroid requires certain ingredients to manufacture T3 and T4 hormones and to convert T4 to its active form T3 – including:
- Raw materials iodine and tyrosine (an amino acid)
- Thyroglobulin (Tg), Thyroperoxidase (TPO) enzyme and hydrogen peroxide – produced inside the thyroid follicles, the Tg protein molecule converts iodide to iodine via TPO enzyme (mediated by H2O2) for incorporation with amino acid tyrosine residues, to be used for making thyroid hormones.
- Antioxidants and antioxidant-supporting nutrients – including selenium,manganese, and zinc, are necessary to control potentially damaging reactive oxygen species (ROS), inherently created in TH production and activation processes.
Support nutrients required for thyroid hormone production
Problems occur when the thyroid produces too many or too few thyroid hormones
- Excessive thyroid hormone production (called hyperthyroidism) – an overactive thyroid can increase basal metabolic rate (BMR) by 100%.
- Insufficient thyroid hormone production (called hypothyroidism). – an underactive thyroid can reduce BMR up to 50%;
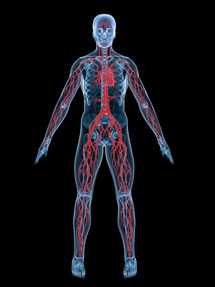
Circulation and transport of thyroid hormones T3/T4
Plasma transport
- Most of the circulating thyroid hormone is bound to transport proteins (70% bound to thyroxine binding globulin (TBG)). Only a very small fraction is free and biologically active. Unbound T4 (fT4) = 0.03%; Unbound T3 (fT3) = 0.3%
- When thyroid hormone is bound, it is not active, so the amount of free T3 compared to free T4 is what is important. Thus, measuring total T4 in the blood can be misleading.
Membrane transport of T3 /T4
- Since they are lipophilic (“fat-loving”) molecules, T3 and T4 cross the cell membrane easily and function via a well-studied set of thyroid hormone receptors (receptors in the nucleus of the cell);
- Although they can transverse the cell membrane in a passive manner, at least 10 different active, energy dependent and genetic regulated iodothyronine transporters have been identified in humans. They guarantee that intracellular levels of thyroid hormones are higher than extracellular blood plasma or interstitial fluids (tissue fluids).
References
http://www.medicinenet.com/script/main/art.asp?articlekey=18395














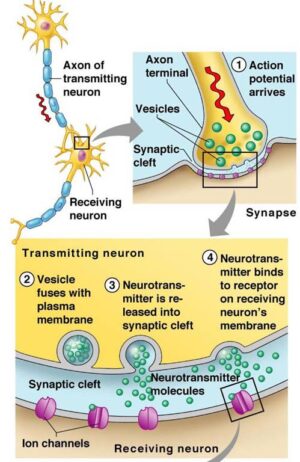
![<span class="ACETYLCHOLINE">Acetylcholine (Ach)</span><span class="hdg-smaller"> – Movement, memory, learning neurotransmitter</span> – [Cloned #60543]](https://healthhappening.com/wp-content/uploads/2025/12/Ach.jpg)