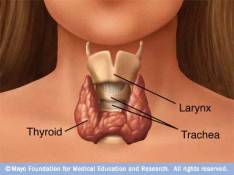
Thyroiditis - Inflammation of the thyroid gland
Thyroiditis is the result of an attack on the thyroid gland
An attack causes inflammation, damage and possible death of thyroid gland cells (thyrocytes).
- Thyroiditis may occur because of an autoimmune process, infection, medication, or pregnancy.
- Most types of thyroiditis are 3-5 times more prevalent in women than in men
- Average age of onset is between 30 and 50 years of age
- Tends to be geographical/seasonal. Most common in summer and fall;
- The various types of thyroiditis usually have both hypothyroid and hyperthyroid phases
- Thyroiditis is classified as autoimmune or non-autoimmune depending on the cause of inflammation
Autoimmune thyroiditis
Cause
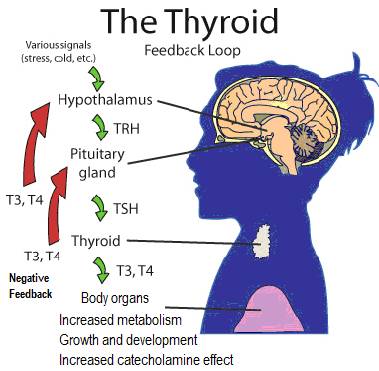
A malfunctioning immune system attack on thyroid cells and tissues promotes a process in which some people make anti-thyroid antibodies. This can lead to thyroid inflammation, tissue damage and disrupted thyroid function
Iodine-deficient patients shown to have higher rate of anti-thyroid antibodies
The anti-thyroid antibodies involved with autoimmune thyroiditis are:
- Anti-thyroid peroxidase (TPO Ab). These antibodies attack the thyroperoxidase enzyme (TPO), responsible for thyroid hormone production.
- Anti-thyroglobulin (Tg Ab). These antibodies block thyroglobulin (Tg), a protein made by the thyroid, necessary for making thyroid hormones (TH)
- TSH Receptor Antibody (TRAb). These antibodies mimic TSH and stimulate thyroid hormone production by binding to thyroid stimulating hormone (TSH) receptors.
And possibly:
- Na+/I- Symporter (NIS) Antibody – the NIS transports iodide into the thyroid follicular cell and this antibody is present in 20% of Grave’s disease and 26% of Hashimoto’s thyroiditis. Saravanan P, Dayan CM (June 2001). “Thyroid autoantibodies”.Endocrinol. Metab. Clin. North Am: 315-37, viii..I
Immune system attack on thyroid ==> anti-thyroid antibodies ==> Increased or Decreased thyroid hormone (TH) production
Thyroid problems can develop when anti-thyroid antibodies damage thyroid gland components resulting in a malfunctioning thyroid – which either (1) Decreases or (2) Increases thyroid hormone production:
- Antibody against TPO (TPOAb) – These antibodies damage the TPO enzyme responsible for adding iodine to thyroglobulin protein in thyroid hormone (TH) production; usually a consequence of iodine and/or selenium deficiencies; high TPO Ab found in ~90% of patients with Hashimoto’s thyroiditis.
- Antibodies against thyroglobulin (TgAb) – These antibodies block thyroglobulin (Tg),a protein synthesized by the thyroid, required for making thyroid hormones (T4 and T3). High TgAb levels seen in patients with Hashimoto’s thyroiditis.
- Also, women’s high level TgAb linked to Infertility / miscarriage (for currently unclear reasons), TgAb can interfere with implantation of the embryo in the uterus.
- TSH Receptor Antibodies (TRAb) – These antibodies mimic TSH and stimulate thyroid hormone production by binding to thyroid stimulating hormone (TSH) receptors. Found in ~95% of those with Grave’s hyperthyroidism.
CHART OF ANTI-THYROID ANTIBODIES and Associated thyroid DISEASES | |||
ANTI-THYROID ANTIBODIES | ACRONYM | EFFECT ON TH PRODUCTION | PRESENT IN |
Anti-thyroid peroxidase (TPO) antibody | TPOAb | ▼▼▼ | Autoimmune Thyroiditis (E.g. Hashimoto’s thyroiditis (found in ~90% of cases), Postpartum thyroiditis) Graves’ Disease (found in ~75% of cases) |
| Anti-thyroglobulin antibody | TgAb | ▼▼▼ | Thyroid cancer; Autoimmune Thyroiditis (E.g. Hashimoto’s thyroiditis, Postpartum thyroiditis) |
| Anti-Thyroid Stimulating Hormone (TSH) receptor antibody | TRAb | ▲▲▲ | Graves Disease (found in ~95% of cases) |
Autoimmune thyroiditis includes:
Hashimoto’s disease (aKA. lymphocytic or autoimmune thyroiditis)
- Most common cause of hypothyroidism in N. America. First described by Dr. Hakuru Hashimoto in Japan, 1912.
- Life-long autoimmune disease. The thyroid gland is gradually destroyed by a variety of cell and antibody-mediated immune processes causing permanent hypothyroidism; Both TPO Ab and Tg Ab are elevated in most Hashimoto’s cases. The inflamed gland causes it to swell.
- Occurs more often in women than in men (between 10:1 and 20:1). Most prevalent between 45 and 65 years of age; an average of 1 – 1.5 in a 1000 people have this disease;
- Often results in hypothyroidism with bouts of hyperthyroidism.
Postpartum thyroiditis
- Diffuse goiter usually present. Typically 1.5 – 3 times normal gland size
- Affects ~5% of women within a year of giving birth and is an exacerbation of an underlying autoimmune thyroiditis. Aggravated by the immunological rebound that follows the partial immuno-suppression of pregnancy.In essence, the immunological rebound that follows the end of pregnancy precipitates the clinical expression of Hashimoto’s disease, which before pregnancy was clinically silent. Muller AF, Drexhage HA, Berghout A. Postpartum thyroiditis and autoimmune thyroiditis in women of childbearing age: recent insights and consequences for antenatal and postnatal care. Endocr Rev. 2001 Oct;22(5):605-30. PubMed
- First Phase. Hyperthyroidism occurs 1-4 months after delivery, lasts only 2-4 months. Of those with postpartum thyroiditis in the hyperthyroid phase, 25% are found to have TRAb antibodies and ~80% have a positive test result for TPO Ab. Associated symptoms include anxiety, insomnia, palpitations (fast heart rate), fatigue, weight loss, and irritability. This phase of postpartum thyroiditis can be confused with Grave’s disease. When present, either exophthalmos (bulging eyes) or a thyroid bruit (audible sound of increased blood flow over hyperactive gland) confirms Graves’disease. After the hyperthyroid phase, the thyroid then returns to normal or progresses to:
- Second phase. Hypothyroidism 3-9 months after child-birth; typical symptoms include fatigue, weight gain, constipation, dry skin, depression and poor exercise tolerance. Most cases resolve after about 12-18 months, but 1 in 5 of these women will develop permanent hypothyroidism.
Silent / painless thyroiditis (aKA. subacute lymphocytic thyroiditis)
Tends to have a phase of hyperthyroidism / thyrotoxicosis (excess thyroid hormones) followed by a return to normal, and then a phase of hypothyroidism, followed again by a return to normal. The time span of each phase can vary, each typically lasting 2-3 months. During the hyperthyroid phase, iodine uptake is suppressed, while during the hypothyroid phase, uptake is increased. This is different to the elevated iodine uptake found in those with Grave’s disease.
Non-autoimmune thyroiditis
Caused by infectious microbes (E.g. bacteria, viruses). Includes:
Acute infectious thyroiditis
- Mainly bacterial infection, but any microbial infection. Works in the same way as antibodies to cause inflammation; uncommon form of thyroiditis; occasionally painful; mild hypothyroiditis
Subacute thyroiditis (also called de Quervain’s thyroiditis)
- Presumed caused by a virus (often follows an upper respiratory infection). Can be a cause of hypothyroiditis and painful hyperthyroiditis / thyrotoxicosis; different to post-partum and silent thyroiditis in that this type is associated with pain (usually in hyperthyroid phase); Also, may trigger autoreactive B cells to produce TSH (thyrotropin) receptor antibodies (TRAb), resulting in TRAb-associated thyroid dysfunction in some patients. Iitaka, M, Momotani, N, Hisaoka, T, Noh, JY, Ishikawa, N, Ishii, J, Katayama, S Ito, K 1998 TSH receptor antibody-associated thyroid dysfunction following subacute thyroiditis Clin Endocrinol (Oxf) 48 :445-453. PubMed
Chronic infectious thyroiditis
- Usually caused by a fungus in those with weakened immune system. Mild tenderness occurs on both sides of thyroid. May lead to hypothyroidism. Kenneth Burman, MD, Overview of thyroiditis
Caused by toxic substances
Drug-induced thyroiditis
- Drugs such as lithium, amiodarone (cordarone – high iodine content, used for arrhythmia), interferon-alpha and cytokines have a tendency to damage thyroid cells. Can lead to either thyrotoxicosis (excess thyroid hormone) or hypothyroidism;
- Radiation exposure follows treatment with radioactive iodine for hyperthyroidism, or external beam radiation therapy for certain cancers. This frequently leads to hypothyroidism, and occasionally thyrotoxicosis (excess presence of thyroid hormone).
Symptoms of thyroiditis
Thyroiditis can cause slow, long-term damage to thyrocytes that cause blood thyroid hormone levels to fall ▼▼▼. If this happens, symptoms are similar to hypothyroidism (under-active thyroid) :
| Symptoms of Hypothyroidism | |
|---|---|
| May include: | |
| Feeling constantly fatigued | Aching muscles / Vague aches and pains |
| Cold hands and feet | Weight gain without eating more |
| Coarse, dry, thinning hair | PMS /Heavy menstrual periods / menstrual cramps |
| Dry skin | Forgetfulness |
| Slow heartbeat | Loss of libido |
| Mental sluggishness/”Fuzzy headed” | Constipation |
| Depression | Pain in thyroid gland (at front of neck) |
| Low basal temperature | Infertility /anovulatory cycles / repeated miscarriage |
| Slowed knee-jerk reflexes | |
Thyroiditis can cause rapid thyroid cell damage / destruction that causes thyroid hormone in the gland to leak out and so increase the blood thyroid hormone levels ▲▲▲. This causes symptoms similar to hyperthyroidism (over-active thyroid). The excess presence of thyroid hormones is referred to as thyrotoxicosis.
| Symptoms of HYPERthyroidism | |
|---|---|
| Typical Symptoms Include: | |
| Weight loss -despite increased appetite | Nervousness, Anxiety, irritability |
| Heat intolerance | Tremors in hands/fingers |
| Muscle weakness/aches | Fatigue |
| Excessive production/excretion of urine (Polyuria) / Excessive thirst | Hyperactivity |
| Apathy | Hypoglycemia |
| Non-pitting edema over the shin (Pretibial myxedema) | Sweating |
| Can also include: | |
| Palpitations/ increased heart rate / arrhythmia | Memory loss |
| Diarrhea | Insomnia |