Skin cancer- Most common form of cancer

Skin cancer is the most common form of cancer in the U.S. and can occur anywhere on the body, but most commonly occurs in skin often exposed to sunlight. E.g. the face, neck, and hands. It especially occurs in fair-skinned and fair-haired people, those who had freckles as a child and those who have blue eyes.
Skin
Has several functions
- Protection from environment. Uv-radiation, chemicals, such as in soaps and lotions, oxidants, microbes
- Keeping cool. Sweat glands secrete sweat
- Prevents water loss when necessary
- Communication. Nerve fibers carry sensation to / from brain, such as when you touch that hot pan.
- Nutrient storage. For healthy skin
- FIbroblasts synthesize collagen and elastin
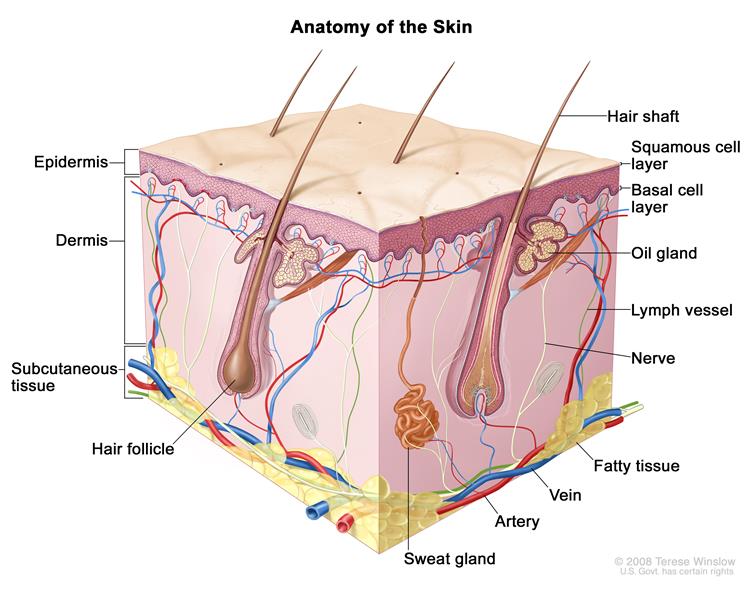
The epidermis - our barrier to the world
The thickness of a sheet of paper, varies somewhat according to site, the epidermis is the topmost layer of our skin, and the first line of defense against the air and UV light, constantly subjected to damage from oxidative stress. Its main cell types are:
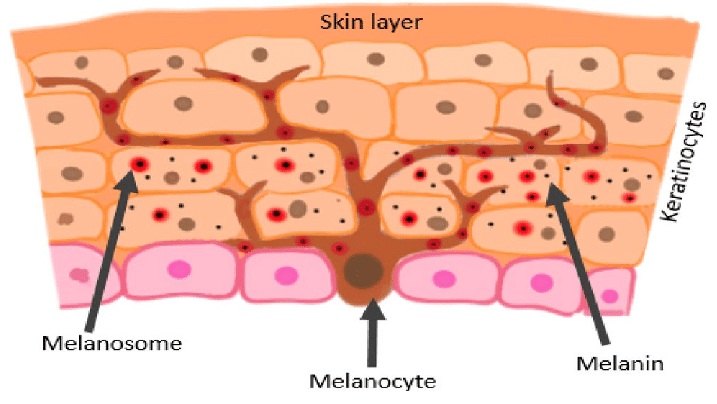
- Keratinocytes – skin cells that accumulate the protein keratin as they move outwards to form a dead, hardened, impermeable layer, which eventually rubs or sloughs off.
- Melanocytes – produce melanin (pigment), which is packaged into melanosomes and transferred to keratinocytes.
- Dendrocytes (Langerhans cells) – antigen-producing immune cells, help remember and recognize new allergens (substances foreign to body).
- Merkel cells – responsible for light, touch and sensation; plentiful in sensitive skin. Make synaptic contact with somatosensory afferent nerve fibers. Merkel cell carcinoma is a rare but aggressive cancer.
The dermis
The dermis is less dense than the epidermis. It contains connective tissue, blood vessels, oil and sweat glands. nerves, hair follicles, and other structures.
Its main cell types are:
- Fibroblasts. Synthesize and organize structural proteins such as collagen and elastin.
- Immune cells, such as monocytes, macrophages and dermal dendrocytes, which modulate response to injury.
Subcutaneous tissue (Hypodermis)
This layer hosts fat, connective tissues, large blood vessels and various nerves. Its primary function is to insulate the body to regulate body temperature

Who is most at risk for skin cancer?
Those who have:
- Light skin, blond or red hair and / or light-colored eyes
- Freckles
- 50 or more moles
- Family history of skin cancer
- Sun sensitivity
- > 5 sunburns.(doubles risk)
- A history of prolonged unprotected, outdoor UV-exposure (especiallly if fair-skinned)
- A history of using tanning beds
- Atypical moles
- Reduced immune system function

Squamous cell carcinoma (SCC)
Flat squamous cells form the outermost layer of the epidermis. Squamous cell carcinoma (SCC), a.k.a. “rat-bite” tumor, is diagnosed when these cells become abnormal and grow out of control. SCC sometimes develops from a precancerous skin growth called an actinic keratosis. SCC is usually seen as scaly red patches or open sores, which may crust and bleed. Characteristically it looks elevated with a central hole. Allowed to grow, it can be fatal.
Bowens disease is a form of squamous cell cancer in situ.

Basal cell carcinoma (BCC)
Basal cell carcinoma is the most common type of cancer in the U.S. and the most common skin cancer. 90% of the epidermal cells, so named because they are found in its basal layer, below the squamous cells. These round cells are also called keratinocytes. BCC is usually benign i.e. a relatively harmless skin cancer. It typically looks like a red patch, scar, shiny bump, pink growth or an open sore, which can bleed, ooze or crust. Rarely spreads or metastasizes, but should not be ignored since it is more easily treated whilst small.

Melanoma
In situ and invasive
Melanoma is a skin cancer involving the uncontrolled growth of melanocytes (cells In the lower epidermis of the skin, that produce melanin) – the pigment that gives skin its color, made darker when exposure to the sun triggers melanocytes to make more melanin pigment to absorb UV rays to protect the skin. The difference between melanoma in situ and invasive melanoma is the extent of its growth. Melanocytes are synthesized by melanosomes.
Melanoma begins in the skin’s outer layer, called the epidermis, occurring in such as back, neck, arms, legs, scalp, face, soles of feet and palms. Melanoma can also occur in other areas of the body, such as the mucous membranes accounting for 1.4% of melanoma.(incidence rates have been stableover time,non-keratinized and moist, inside mouth, nose, vagina, anus), and eyes (called occular melanoma), and just about anywhere in the body if it becomes invasive.
Melanoma in situ. In initial stage 0 melanoma is in the epidermis (thin top layer) of skin and stays in situ.. 1.4% of melanoma.
Invasive melanoma. Stages 1 – 4 are called invasive melanoma, with each stage going deeper. At stage 3, it has penetrated the basement membrane to enter the lower level of skin, called the dermis. With access to lymph tissue, blood vessels and nerves, the melanoma cells can travel to body organs, such as liver or lungs, distant lymph nodes, and the central nervous system, at which point it is defined as stage 4 / metastatic melanoma. Catching melanoma in its early stages is crucial, since the 5 year survival rates are around 99% for stages 0,1, and 2 but drop dramatically to ~75% for stage 3 and ~35% for stage 4
Causes of melanoma
DNA in melanin-producing cells becomes damaged, which if not repaired by the immune system, causes cells to multiply out of control forming malignant tumors. Study in 2020 reported >90% of melanoma cases in the United States are attributable to UV radiation, affected by UV index and geographical location.
- UV radiation from tanning beds can induce DNA damage.
- Non-UV-mediated melanoma is less common and can occur in sun-protected sites, such as the soles of the feet, palms, in the mouth, in nasal mucous membranes or under the nails. Existing moles are responsible for only 29% of melonoma origin, while 71% begin in new spots. PubMed
The sun can damage DNA in skin cells, which if not repaired by the immune system, can cause skin cells to multiply rapidly and form malignant tumors. Curable if detected early, but each year in the U.S. ~8,000 people die of this type of cancer (2023), the most fatal of cutaneous cancers. Here’s the interesting fact though – a significant percentage of melanoma, sometimes aggressive, is not related to UV radiation, and can even occur in places where the sun doesn’t shine.
Melanomas are not always dark colored. Rarely, they can be pink or skin-colored. Watch out for a spot on the skin that looks different to other spots – the “ABCDE” signs, which may indicate melanoma, but not all have to be present:
- Asymmetrical: a line drawn through the middle of a tumor produces relatively similar halves;
- Border: irregular or jagged, not smooth. May fade into surrounding skin.
- Colored: A combination of colors is usual. Invasive melanoma has multiple brownish shades from light tan to dark black. Regression is indicated as areas turn lighter or white. Increased inflammation and increased blood vessels may redden area. Benign tumors are more likely to be one color.
- Diameter > 1/4 inch: non-malignant skin cancers tend to be smaller
- Evolving: Grows notably in elevation and diameter / Gains more colors, and can itch (but not always a symptom) or bleed. Can become a dome-shaped nodule (called nodular melanoma). As surface cells are damaged, the tumor becomes ulcerated and its surface may break down with oozing or crusting. Non-cancerous moles stay the same size and color or change slowly.
In uveal melanoma – the role of ultraviolet (UV) light is more controversial, but likely contributes to at least a subset of cases
Non-UV-mediated melanoma (in places where the sun doesn't shine)
Cause of DNA damage is not usually UV light. What is causing the damage is still under investigation – could be related to trauma.
Mucosal melanomas. Occur on mucus membranes on cavities exposed to the outside of the body, inside the nose, mouth, rectum, eyelids, and vagina. These melanomas are not caused by direct UV exposure.
- Melanoma in the mouth (accounts for almost half of mucosal melanomas). Can manifest as mouth ulcers, unexplained nosebleeds, and a lump in the neck, jaw, or mouth, with possible visible lesions, mouth pain or inability to talk
- Melanoma of the anus. Manifests as possible anal bleeding, a protruding growth / lump, constipation, pain / discomfort.
- Melanoma of vagina or vulva. Can be experienced as unexpected vaginal bleeding, a mass felt inside vagina, or visible lesions on vulva, with pain / discomfort
Acral (means extremity) lentiginous melanoma (ALM) is a subtype of cutaneous melanoma (lentiginous means the melanoma spot is darker than the skin surrounding it and has a sharp border presenting a stark contrast to the lighter skin around it). ALM most commonly occurs on palms or soles of feet, and can also occur under the finger or toenails (called subungual AM), in which discoloration (general, spots or lines) extends to the cuticle and can cause the nail to crack or break in its advanced stage. ALM may stem from physical stress / injury, suggested by its propensity for the bottom of the feet, which undergo pressure from weight or tight shoes or wearing high heels. PubMed Subungual hematomas are when an injury causes blood to be trapped under the nail and looks different to subungual melatoma in that it looks more like a dark smudge or bruise under the nail. ALM represents only 2-3% of melanomas in Western populations, but is the most common type of melanoma in non-Caucasians with darker skin (namely those of Hispanic, African, or Asian heritage). In Asian countries such as Taiwan, China, Japan, Korea, Hong Kong, and Singapore, AM has been reported to account for up to 58% of all melanomas. PubMed

Melanoma under the nail. Watch for a dark band > 3mm in width or a spot that looks fuzzy around the edges.

Essential fats prevent skin cancer
Essential fats (Omega-3 and Omega-6)
- Electron clouds of essential fatty acids residing in skin cell membranes resonate with and absorb UV rays
- Omega-3 has an important role in restoring skin damage caused by UV-B. A study exposing mice to UV-B found that Omega-3 in their diet reduced epidermal damage caused by UV-B and suppresses excessive epidermal water loss (UV-B typically disrupts the stratum corneum’s ability to retain water – whose moisture is an anti-inflammatory protection against environmental stress). The stratum corneum is the outermost layer of the epidermis.
- Essential fats produce eicosanoids, potent local “first responders” mediating inflammation in response to skin damage

Skin cancer treatments
BCC, SCC and melanoma in situ (stage 0) skin cancer treatment choices
- PEMF therapy using SOTA Magnetic Pulser (Applied over cancerous area)
- Ozone Therapy (Ozonated olive oil (OOO); Ozone Funneling)
- Chlorine Dioxide Therapy (CDT) – Applied externally using DMSO
- Black Salve
- 7% Iodine Tincture
- Topical eggplant extract. Used since 1825, eggplant extract has been shown to be effective in the treatment of both malignant and benign human skin tumours. Solasodine rhamnosyl glycosides (BEC) can be extracted from eggplants. A preparation (Curaderm™) which contains 0.005% BEC is effective in the treatment of keratoses, basal cell carcinomas (BCCs) and squamous cell carcinomas (SCCs) of human skin. Link
- Topical myrrh and frankincense essential oils. DIluted in carrier oil and rubbed on lesions shown effective against skin cancers. Myrrh is rich in sesquiterpenoid and curzerene. Frankincense has several active ingredients. Link?
- DMSO. Has shown promising results for basal cell carcinoma. Dimethyl sulfoxide (DMSO): a solvent that may solve selected cutaneous clinical challenges – PubMed

Stage 4 melanoma

(1) Cancer Treatment Core
Of special mention
Baking soda / Maple Syrup Protocol. Baking soda alkalizes cells. Researchers have found that this protocol inhibits malignant growth by increasing tumor pH, and also reduces formation of spontaneous metastases. The sudden pH increase kills the cancer cells. as the shock of alkalinity allows more oxygen into the cancer cells than they can tolerate. (OR If, like this author,you hold with the microbial theory of cancer, it causes cancer microbe inside cells to die or go into its hibernating form, such that cells revert to normal metabolism. Baking Soda / Maple Syrup against Cancer
Magnesium. Magnesium against Cancer Without sufficient magnesium, the body accumulates toxins and acid residues and degenerates rapidly. For any degenerative disease, especially cancer, transdermal or nebulized magnesium chloride is a “No-brainer” to quickly build up the body’s magnesium levels.
(2) Eliminate cancer cells
Treatment options: depend on the stage of cancer development and your choices are presented in the:

References
Chang KJ, Lee TTY , Linares-Cruz G, Fournier S, de Lignieres B (1995) Influences of percutaneous administration of estradiol on human breast epithelial cell cycle in vivo. Fertility and Sterility; 63; 7865-7891. Online link
Collaborative Group on Hormonal Factors in Breast Cancer. Familial breast cancer: collaborative reanalysis of individual data from 52 epidemiological studies including 58,209 women with breast cancer and 101,986 women without the disease. Lancet. 2001;358(9291):1389–1399. PubMed
Ikram Ullah, Govindasamy-Muralidharan Karthik, Amjad Alkodsi, Una Kjällquist, Gustav Stålhammar, John Lövrot, Nelson-Fuentes Martinez, Jens Lagergren, Sampsa Hautaniemi, Johan Hartman, Jonas Bergh (2018) Evolutionary history of metastatic breast cancer reveals minimal seeding from axillary lymph nodes. Journal of Clinical Investigation; DOI: 10.1172/JCI96149
Ullah I, Karthik GM, Alkodsi A, Kjällquist U, Stålhammar G, Lövrot J, Martinez NF, Lagergren J, Hautaniemi S, Hartman J, Bergh J. Evolutionary history of metastatic breast cancer reveals minimal seeding from axillary lymph nodes. J Clin Invest. 2018 Apr 2;128(4):1355-1370. doi: 10.1172/JCI96149. Epub 2018 Feb 26. PMID: 29480816; PMCID: PMC5873882. PubMed
Hormone-sensitive breast cancer studies
Mohammed, Hisham, et al (2015) Progesterone receptor modulates ER-a action in breast cancer. Nature ; 523; 313-317. Link.
Perks, Bea (17 Jul 2015) Progesterone receptor could slow breast cancer growth. Pharmaceutical Journal. Link.
Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, Jackson RD, Beresford SA, Howard BV, Johnson KC, Kotchen JM, Ockene J (2002 Jul 17) Writing Group for the Women’s Health Initiative Investigators. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women’s Health Initiative randomized controlled trial. JAMA. 288(3):321-33 PubMed
de Lignières B, de Vathaire F, Fournier S, Urbinelli R, Allaert F, Le MG, Kuttenn F. (2002 Dec) Combined hormone replacement therapy and risk of breast cancer in a French cohort study of 3175 women. Climacteric. 5(4):332-40. Researchgate
Fournier A, Berrino F, Riboli E, Avenel V, Clavel-Chapelon F. (2005 Apr 10) Breast cancer risk in relation to different types of hormone replacement therapy in the E3N-EPIC cohort. Int J Cancer. 114(3):448-54. PubMed
Laura P. Stabile, Autumn L. Gaither Davis, Christopher T. Gubish, Toni M. Hopkins, James D. Luketich, Neil Christie, Sydney Finkelstein and Jill M. Siegfried. Human Non-Small Cell Lung Tumors and Cells Derived from Normal Lung Express Both Estrogen Receptor α and β and Show Biological Responses to Estrogen. Cancer Res April 1 2002 (62) (7) 2141-2150; Link