How does the thyroid produce hormones?
For those wanting more detail: Thyroid production in detail
The thyroid follicles - T4 / T3 thyroid hormone production site

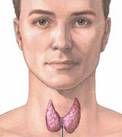
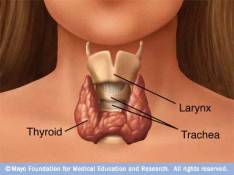
The functional units of the thyroid gland are spherical follicles – balls of follicular cells with hollow centers, each follicle consists of:
- Thyroid follicular cells (simple cuboidal type, aka. thyroid epithelial cells, follicular epithelial cells, thyrocytes); form the outside boundary . . .
- Filled with a viscous material called colloid – which contains mostly glycoprotein thyroglobulin (Tg) molecules, that provide:
- The glycoprotein backbone for synthesis and storage of thyroid hormones
- A convenient depot for iodine storage and retrieval – when external iodine availability is scarce or erratic.
Iodine + Amino acid tyrosine → T3 and T4.
Thyroid hormone (TH) production of Thyroxine (T4),Triiodothyronine (T3) is a complex process taking place in the thyroid follicles. Its main steps are:
- Stimulation by thyroid stimulating hormone (TSH) secreted by the pituitary gland
- Iodide transported from the blood stream to the follicular lumen – iodide is concentrated to about 30 times blood concentration via the Sodium/Iodide pump (NIS)
- Thyroglobulin (Tg) is produced and secreted inside the thyroid follicular cell stimulated by TSH – and then Tg travels to the follicular lumen where it is used to form thyroid hormones
- Iodide is oxidized to iodine – via the thyroperoxidase enzyme (TPO), mediated by hydrogen peroxide (H2O2)
- iodine is incorporated within thyroglobulin (thyroglobulin iodination) for the production of TH intermediates. Catalysed by TPO, Iodine is incorporated into tyrosyl (amino acid tyrosine) residues in theTg molecule and formed into iodotyrosines MIT and DIT (thyroid hormone intermediates)
Formation (MIT / DIT coupling) and storage of thyroid hormones in follicle colloid – MIT and DIT (products of Tg iodination) are bonded via TPO to make the thyroid hormones T3 (1 MIT + 1 DIT) and T4 (2 residues of DIT), where they can be stored for up to 3 months in the colloid of the follicular lumen, as part of thyroglobulin. This storage form is called follicle colloid.
- MIT + DIT → T3 (3 iodides) Via TPO
- DIT + DIT → T4 (4 iodides) Via TPO
- When needed, TSH stimulates release of T3 and T4 – thyroid hormones are reabsorbed from the colloid in the follicular lumen into the follicular cells, where they are cleaved from thyroglobulin (Tg) and released into circulation
Importance of appropriate iodine supply for making thyroid hormones
- Too much or too little iodine impairs adequate TH synthesis – as at any factory, effective production depends on three key components – adequate raw material (T4 is 65% iodine by weight), efficient machinery, and appropriate controls. Like many things in life, the amount of iodine required for a smooth operation has a “Goldilocks” factor – too much or too little available iodine detrimentally affects the auto-regulation of T3 / T4 synthesis, and in either case can cause goiter (a swollen thyroid gland).
For more detailed information on thyroid hormone production:
Thyroid Hormone Production – In detail
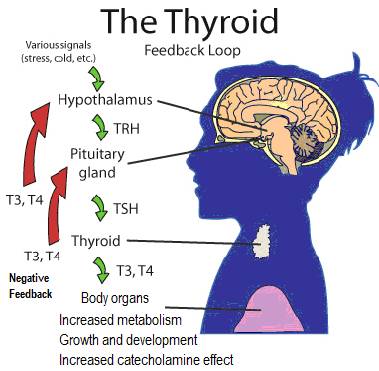
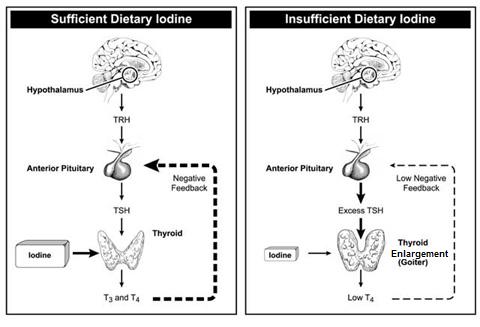
Thyroid production feedback loop
Thyroid’s T4/T3 production is controlled by hypothalamic control of the pituitary gland’s production of thyroid stimulating hormone (TSH), by negative feedback of T3/T4 levels
The hypothalamus in the brain releases TRH (Thyrotropin-Releasing Hormone) – to modulate the pituitary gland’s release of TSH (Thyroid Stimulating Hormone);
TSH circulating in the bloodstream tells the thyroid to make T3 and T4 thyroid hormones – and release them into the bloodstream, to be converted as needed to T3, mainly by the liver;
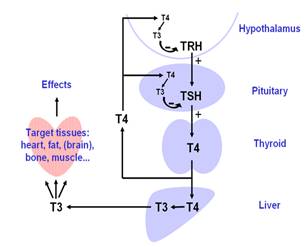
The pituitary gland’s TSH production is sensitive to the T3/T4 levels in the blood
- When the T3/T4 levels drop, the pituitary produces and releases more TSH. This stimulates the thyroid to make more T4 and T3 thyroid hormones and release them into the bloodstream;
- As the thyroid hormone levels rise, the pituitary reduces or shuts off TSH. This negative feedback mechanism keeps the level of thyroid hormones in a fairly constant range with a normally-functioning thyroid.
TSH production is also reduced by:
- Somatostatin – hormone that inhibits secretion of growth hormone
- Rising levels of glucocorticoids and sex hormones (e.g. Estrogen, TESTOSTERONE)
- Excessively high blood iodide concentration – as a self protecting mechanism.
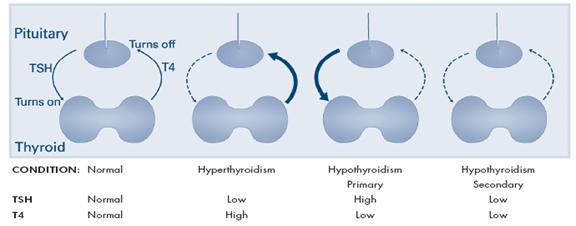
TSH-T4 level conditions
- Stress
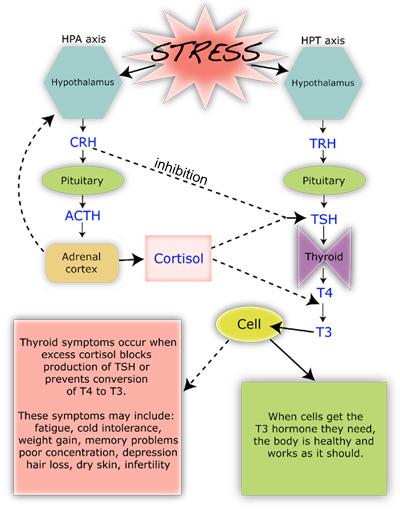
Stress Affects TH production and T4 to T3 Conversion
Neither TSH or blood Plasma T3/T4 Levels alone are a substantive evaluation of thyroid function
The level of thyroid hormone (i.e. T3 and T4) production is determined by:
- Levels of TSH released from the pituitary gland – producing a feedback loop so that TSH increases as thyroid hormones decrease, and TSH decreases when thyroid hormones increase;
- AVAILABILITY of IODINE and TYROSINE (converted by the thyroid to the thyroid hormones) – Insufficient iodine causes thyroid cell enlargement (hypertrophy), leading to an enlarged thyroid (goiter).
Iodine Availability
- The condition of the thyroid tissues themselves;
- Further regulated by the hypothalamus, by other nutrient requirements, and no doubt other regulatory mechanisms
TSH level is also NOT a reliable indicator of thyroid function for many people.
- Low amounts of T4 in the blood, due to lack of dietary iodine to make them, gives rise to high levels of TSH;
- A low TSH level should indicate optimum or high thyroid hormone levels, however, the TSH level simply indicates how much T4 the pituitary is getting, and . . .
- The thyroid may be producing enough T4 (keeping TSH low), but the body isn’t converting enough available T4 to T3
- The pituitary and the hypothalamus(which controls the pituitary) may not be functioning optimally