Clinical and simple DIY tests for thyroid metabolism

Simple “Do-it-yourself” tests to determine thyroid function
Involves taking your basal temperature for 5 days or measuring urine temperature:
(1) Barnes Basal Temperature Method
Developed by Broda O. Barnes, M.D., author of Hypothyroidism: The Unsuspected Illness as long ago as 1942. Not definitive, but provides a good indicator of potential hypothyroidism.
- Obtain a Basal / Fertility Thermometer (accurate to within 0.1 degrees, compared to a standard thermometer which is only accurate to within 0.2 degrees). A digital Basal Thermometer is less than $10 at your local pharmacy.
- Place the thermometer on your nightstand – for immediate access when you wake up in the morning. Do not use an electric blanket.
- Upon awakening place the thermometer snuggly in your armpit – this axillary temperature is more accurate than oral, since it is less affected by sinus and oral infections;
- Make sure you give the thermometer plenty of time to accurately measure your temperature (10 minutes is generally recommended for a basal thermometer – Refer to the instructions that came with your thermometer) – It is important that you don’t get out of bed and remain as still as possible until you have read your temperature. (basal temperature reads about 0.5 -1 °F less than oral temperature)
- Take your temperature each morning for 5 days.
- For women who are menstruating – start on the third day of menstruation (Menstruating can lower basal temperature).
- For men and postmenopausal women – it makes no difference what day you start.
If your average temperature is :
- 97.8°F – 98.2°F – your thyroid function appears to be normal.
- Below 97.3°F – suspect a low thyroid metabolism problem, or possibly hypoadrenal function.
Menstruation and illness can elevate temperature
(2) Confirming clinical hypothyroidism
(Test normal for T3, T4, TSH, but experiencing hypothyroid symptoms)
Another reliable way to confirm clinical hypothyroidism is to measure your urine temperature for 3 consecutive days
- Immediately on rising in the morning, urinate into a styrofoam cup
- Measure urine temp. with an ordinary health thermometer
- Continue for 3 consecutive days (if you forget a day, start again).
If the temperature is consistently below 98.6 (usually 97), then you most likely have clinical hypothyroidism.
Clinical tests to determine cause of thyroid dysfunction
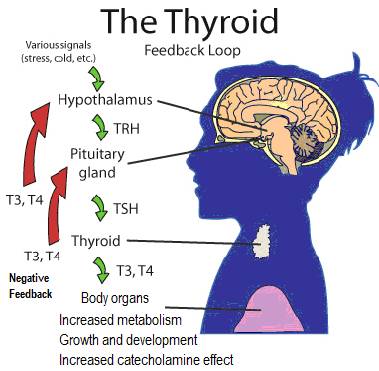
The following tests can determine whether a problem is in the pituitary (related to aging), the thyroid (related to development of systemic antibodies), or a mineral and/or vitamin deficiency (E.g. iodine, selenium, calcium, magnesium, antioxidant vitamins A, D, E and C).
- Thyroid stimulating hormone (TSH)
- freeT4
- free T3
- Thyroid Binding Globulin (TBG)
- Reverse t3 (rT3)
- Antibody Tests
Thyroid stimulating hormone (TSH)
Normal TSH Adult Levels – 0.4 -4.5 mIU/L or mU/L; (recently lowered to 3.0)
High TSH may be caused by:
- An underactive thyroid gland (hypothyroidism) – Hashimoto’s thyroiditis is the most common cause of primary hypothyroidism;
- Pituitary gland making too much TSH – uncommon;
Low TSH maybe caused by:
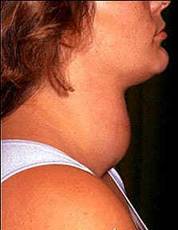
- An overactive thyroid gland (hyperthyroidism) – usual causes are Grave’s Disease, a toxic multinodular goiter (Plummer disease, enlarged thyroid) or a toxic nodule (a non-cancerous tumor);
- Damage to pituitary gland – preventing it from making TSH, called secondary hypothyroidism;
- Pregnancy during 1st trimester
The designated TSH high level is too low –this figure was determined in 1973 from a sampling of volunteers that did not exclude those with a family history of hypothyroidsm. As a result people can test with a “satisfactory” TSH, but still demonstrate hypothyroid symptoms
- Rather than testing TSH, a better approach is to look for:
- Elimination of symptoms
- A mid-afternoon temperature of 98.6 (using a mercury thermometer) – while maintaining a normal heartrate
- Getting free T3 in the normal range – together with healthy adrenal function
free t4
Measures AVAILABILITY of thyroxine (represents 75% of thyroid hormone) – only unbound hormone (not attached to TBG binding protein in blood) is easily bioavailable;
Normal Adult T4 Levels – 4.5 to 11.2 mcg/dL;
High T4 along with low TSH levels –may be due to conditions involving an overactive thyroid:
- Early Hashimoto’s thyroiditis
- Grave’s disease
- High levels of hormone-binding protein Thyroid Binding Globulin (TBG) – can occur with pregnancy, birth control use, estrogen dominance, liver disease;
- Iodine-induced hyperthyroidism;
- Subacute or chronic thyroiditis;
- Toxic multinodular goiter
- Gestational trophoblastic disease – a group of rare tumors that involve abnormal growth of cells that start in the cells that would normally develop into the placenta during pregnancy;
Low T4 maybe caused by:
- Hypothyroidism;
- Illness
- Malnutrition
- Certain medications – Anabolic steroids, androgens, antithyroid drugs (for example, propylthiouracil and methimazole), interferon alpha, interleukin-2, lithium, Phenytoin, Propranolol
free T3
Measures AVAILABILITY of triiodothyronine (T3) – the active thyroid hormone;
TSH | T4 | T3 | INTERPRETATION |
| High | Normal | Normal | Mild (subclinical) hypothyrodism |
| High | Low | Low or normal | Hypothyrodism |
| Low | Normal | Normal | Mild (subclinical)hyperthyroidism |
| Low | High or normal | High or normal | Hyperthyroidism |
| Low | Low or normal | Low or normal | Nonthyroidal illness; rare pituitary (secondary) hypothyrodism |
Thyroid binding globulin (TBG)
Elevated by estrogen hormone excess
Reduced by androgen excess
Reverse T3 (rT3)
Reverse T3 is the right isomer of T3 (R-T3) – only the left isomer is active (L-T3)
Having high levels of reverse T3 is known as thyroid resistance and produces symptoms of hypothyroidism – a certain amount of rT3 is normal, the problem occurs when the ratio of Free T3 drops in proportion to rT3, allowing rT3 to interfere with T3 energy-production activity. rT3 binds to T3 receptors, which blocks T3 from binding and empowering cellular energy production / metabolism.
About 60% of T4 is converted to its active form T3, but 20% is irreversibly converted to rT3 – Even though it is inactive, its purpose is to lower T3 activity
Levels of reverse T3 are elevated:
- With excessive physical or emotional stress – which first raise CORTISOL ▲ levels to deal with it and then lower CORTISOL levels if adrenals become “worn down”.
- When your body needs to conserve energy to deal with something else (E.g. emotional or physical stress, such as being ill), the excess CORTISOL will increase the amount of T4 converted to RT3 to reduce activation of T3.
- Over time adrenals can become fatigued – and CORTISOL levels either drop to low or alternate between low and high. A low CORTISOL level manifests as chronic anxiety, inability to cope with problems, psychological issues (E.g. paranoia), frequent nausea, light/sound sensitivity, and blood thyroid hormone levels can increase, necessitating the conversion of T4 to excess RT3.
- Also, taking T4-only hormones can cause CORTISOL levels that are too high or too low – as CORTISOL is produced to deal with ongoing hypothyrodism, which ongoing production canlead to adrenal dysfunction / fatigue.
- With low iron levels – Iron is a needed to transport thyroid hormone into the cells, and lack of it can lead to excess thyroid hormone in the blood, which the body then converts to rT3. Adding more T3 will not help.
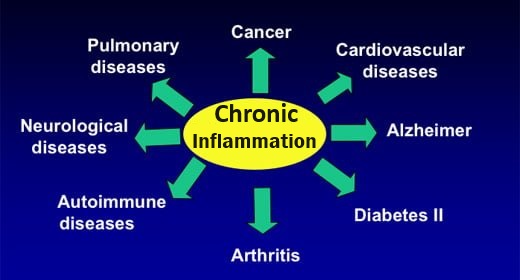
- Many other factors can cause high rT3 – including Low B12 and chronic inflammation.
Antibody tests
Usually ordered to give more information on autoimmune thyroid disease, when TSH, T4 or T3 levels are abnormal.
- TPO (Thyroid peroxidase) antibodies (TPO Ab) – TPO Ab blocks the enzyme TPO responsible for adding iodine to thyroglobulin in TH production.
- Test is read as positive if levels exceed normal range – elevated in 85-90% of those with hypothyroidism (found in most patients with Hashmoto’s hypothyroidism). A positive result indicates an indirect measure of iodine and selenium deficiencies;
- Test is read as negative if normal (i.e. the actual numbers are not important).
- Antithyroglobulin Antibodies (Tg Ab) -These antibodies block thyroglobulin (Tg), a protein made by the thyroid, necessary for making thyroid hormones (T4 and T3).
- Test is positive in patients with Hashimoto’s thyroiditi s – Tg Ab level may also be elevated in other autoimmune conditions such as rheumatoid arthritis, lupus and Sjogren’s syndrome. Tg Ab is used to monitor patients who have had thyroid cancer for recurrence.
- This test should be negative in most patients who have had their thyroid removed.
- Thyroid Receptor Antibodies (TRAb) – tested in those with Grave’s hyperthyroidism. These antibodies stimulate thyroid hormone production by binding to TSH receptors. Thyroid-stimulating immunoglobulin (TSI) and thyrotropin-binding inhibitory immunoglobulin (TBII) are also implicated in Graves disease.