ALLERGIES - Types, symptoms, causes, treatment


What are allergies and who gets them?
An allergy is a chronic over-reaction of the immune system (IS) which can damage normal body tissue
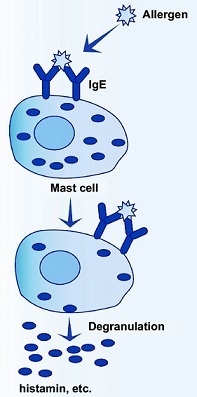
Normally protective components of the IS, antibodies, lymphocytes, and other cells, are involved in allergic reactions and also in autoimmune disease and organ transplant rejection. An allergic reaction usually refers to reactions that involve Immunoglobulin Class E (IgE) antibodies. IgE antibodies bind to certain IS cells, including basophils in the circulation and mast cells (histamine-releasing cells) in the lungs, skin, and mucous membranes.
IgE presence floods your body with inflammatory chemicals, such as histamine and leukotrienes. When IgE antibodies bound to IS cells encounter antigens (called allergens when involved with allergies), the cells are prompted to release chemicals that injure surrounding tissues causing inflammation.
Who gets allergies?
People of any age, but some more than others:
- Women with major depression more likely than women who are not depressed
- More common in men with nervous, anxious (i.e. Type A) personalities
- Those having psychological stress and anxiety – can make seasonal attacks worse and linger longer;
- Allergies tend to run in families, referred to as atopic allergies E,g, atopic dermatitis (eczema)

Types of allergies
Allergy type is determined by the allergen involved – including:
- Plant pollens. In those susceptible to them, they can cause seasonal allergic rhinitis
- Some fungi
- House plants
- Mold (tiny fungal spores) / mildew
- Dust mites / Cockroaches. Eat dead skin in dust, bedding / mattress, furniture, carpet
- Animal / Pet dander (tiny skin flakes from shedding), urine and saliva. Reaction to proteins in animal skin cells, urine or saliva. Cat allergies more common than dogs,
- Industrial chemicals (including tobacco smoke, hair dyes ***)
- Latex. In such as band aids, balloons, rubber bands, latex-based disposable gloves and condoms
- Foods. Commonly peanuts, kiwi
- Medicines
- Perfumes
- Insect venom. Such as from bee or wasp stings; infamous for causing anaphylaxis in some people
- Increased herbicides / GM Soy. Farmers use nearly double the amount of herbicide on GM soy compared to non-GM soy. Higher herbicide residues might cause reactions. GM soy reduces digestive enzymes in mice. If proteins “digest” slowly in humans, there is more time for allergic reactions (possibly to many food proteins).
*** Hair dyes are a common cause of itching and skin rash. Although you can develop an allergy to many ingredients in hair coloring, the chemical Para-diamine (PPD) is the most likely culprit. PPD has been a major component of most hair-coloring products used in the western world since the 1880s and has caused problems almost since it was first developed, according to the American Contact Dermatitis Society–which named PPD as its “allergen of the year” in 2006. Because of its potential to cause an allergic reaction, PPD was banned in Sweden, France and Germany for most of the last century (it re-entered the market after the formation of the European Union). PPD remains popular as a permanent dye because it produces a natural color that doesn’t fade with shampooing.

Allergy symptoms
Most common symptoms
- Sneezing
- A stuffy, runny or itchy nose
- Red, itchy, watery eyes, (called allergic conjunctivitis)
- Postnasal drip. Coughing, caused by a mucus build-up at the back of the throat
- Swelling around the eyes
- A sore throat
- Headache
Sometimes:
- Difficulty breathing / Shortness of breath
- Chest tightness / pain
- Cough
- Wheezing
People with allergies may face an increased risk of panic attacks
A 1995-96 household survey of > 3,000 US adults found that those who reported having hay fever also reported ~twice as many panic attacks.
Anaphylaxis
Potentially life-threatening allergic reaction. Can occur quickly without warning and affect skin, respiration, cardiovascular and digestive systems. The first time you are stung your body produces immunoglobulin E (IgE) antibodies. The next time, the IgE triggers an allergic reaction to the venom.

What causes allergies?
Sinus sensitivity to allergens
Certain people have sensitivity to things in the environment and to the foods they eat. This sensitivity triggers a dilation of blood vessels in the nose and sometimes releases chemicals from cells in the nose that cause swelling. See types of allergens above.
The role of prostaglandins in allergic inflammation
https://www.ncbi.nlm.nih.gov/pubmed/9863413
Hygiene Hypothesis
The hygiene hypothesis proposes that the increase in allergic diseases, including asthma, atopic dermatitis, and atopic rhinitis in many developed countries is through the lack of early exposure to bacteria

Symptomatic treatments for allergies
Mainstream medications for acute or chronic relief
- Antihistamines. Most commonly used
- Intranasal corticosteroids. Effective, but long-term safety is questioned.
- Allergen immunotherapy. Tiny amounts of the allergen are injected under the skin to stimulate immune system production of blocking / neutralizing antibodies that may act to prevent an allergic reaction. Studies show it helps, but cost-effectiveness and risk-to-benefit ratio are factors to consider.
Alternative symptomatic treatments
Moisten sinuses
- Drink plenty of fluids. To thin the mucus (if necessary)
- Use a nasal saline spray. Several times ; do a facial steamday.
- Wash the nose with a salt water solution. From a Neti pot.
- Use a humidifier in rooms where you spend a lot of time. Dry air can irritate sinuses, whereas keeping air moist helps reduce congestion.
- Inhale steam. 2 – 3 times per day (E.g. sit in the bathroom with the hot shower running or do a facial steam over a bowl of hot water with towel over head making a tent)
Eat plenty of a variety of fresh fruits and vegetables.
Especially organically grown, which contain many flavonoids that have anti-inflammatory properties. Found in high concentrations in onions, apples, red wine, broccoli, tea, and Ginkgo biloba. Flavonoid supplements may be helpful, including a combination of quercetin and bromelain, especially if you don’t eat enough vegetables.
- Flavonoids such as luteolin, fisetin and apigenin are inhibitors of interleukin-4 and interleukin-13 production by activated human basophils. We have previously shown that fisetin, a flavonol, inhibits IL-4 and IL-13 synthesis by allergen- or anti-IgE-antibody-stimulated basophils. This time, we investigated the inhibition of IL-4 and IL-13 production by basophils by other flavonoids and attempted to determine the fundamental structure of flavonoids related to inhibition. Due to the inhibitory activity of flavonoids on IL-4 and IL-13 synthesis, it can be expected that the intake of flavonoids, depending on the quantity and quality, may ameliorate allergic symptoms or prevent the onset of allergic diseases. Int Arch Allergy Immunol. 2004.
- Quercetin. This flavonoid is found in a wide variety of vegetables and herbs. In a Japanese study of mast cells from nasal mucosa of individuals with perennial allergic rhinitis, supplemental quercetin significantly inhibited antigen-stimulated histamine release. Quercetin’s effect was almost twice that of sodium cromoglycate at the same concentration.
The recommended quercetin dosage for allergic rhinitis. 250-600 mg, three times daily, five to ten minutes before meals. Gwilliams TG. Allergies: The natural approach The Standard 1998; 1:1-8
Quercetin’s efficacy may be enhanced when taken concomitantly with bromain. Taussig S. The mechanism of the physiological action of bromelain. Med Hypothesis 1980; 6:99-104
- Bromelain. A protein-digesting enzyme from pineapples, increases the absorption of quercetin. Also bromelain alone inhibits several common inflammatory mediators.
Clay Cure for allergies / Hay Fever
The following is an excerpt from Ran Knishinsky’s book, The Clay Cure:
“Allergies and hay fever are caused by the release of histamines. The liver becomes plugged up with toxins and fatty tissue and therefore cannot produce the necessary antihistamines to neutralize the allergic reactions.The first thing to do is clean and rebuild the liver.Once that is done, the allergies and hay fever may disappear.
The good news about clay is that not only will it help stimulate the eliminatory channels, but it can effectively treat allergies and hay fever.Adsorption is a relatively quick process – almost instantaneous in certain cases.The adsorptive surfaces of the clay prevent the allergic reaction by quickly neutralizing allergens before these foreign invaders can attach themselves to the blood cells.In addition, any histamines produced by the allergens that have “gotten away” can also be quickly adsorbed.Water-soluble allergens are bound up by clay because if its intense hydrophilic (water-loving) nature.
Some people, after taking the clay, notice an immediate improvement in their condition.Sometimes the allergies and hay fever disappear altogether.Others see no sudden improvement and must keep taking the clay quite a while before they obtain visible results. The reaction, of course, depends on the state of the liver and the condition of the immune system.A healthier liver will bounce back more quickly than one that is sick.
If you do not achieve results relatively quickly, then give the clay time to work.
One heaping teaspoon once per day in a glass of freshly squeezed lemon water will be sufficient.“
For more information: Medicinal Clays
Vitamin C
Prevents WBC histamine secretion. Murray MT. A comprehensive review of vitamin C. Amer J Nat Med 1996; 3:8-21.
- Histamine levels were found to increase exponentially as plasma ascorbic acid levels decreased. Clemetson CA. Histamine and ascorbic acid in human blood. J. Nutrition 1980; 110:662-668
- Intranasal vitamin C relieves symptoms of perennial AR patients – In a study of the effectiveness of intranasal vitamin C, 48 subjects received either ascorbic acid solution (n=27) or placebo (n=21) sprayed into the nose three times daily. After two weeks 74% of subjects treated with ascorbate solution were found to have decreased nasal secretions, blockage, and edema. Improvement was seen in only 24% of placebo treated patients. The pH of the secretions in the AR sufferers appeared to be more alkaline, over 7.0, with normal nasal secretions tending to be in the range of 5.5-7.0. The pH of nasal secretion was found to be within normal ranges after administration of vitamin C; patients with nasal pH’s closer to 8.0 seemed to respond more favorably to the vitamin C therapy. Podoshin L. Gertner R. Fradis M. Treatment of perennial allergic rhinitis with ascorbic acid solution. Ear Nose Throat J 1991; 70:54-55
- Vitamin C dosage for allergic rhinitis. At least 2 grams per day. Bucca C, Rolla G, Oliva A, Farina JC. Effect of vitamin C on histamine bronchial responsiveness of patients with allergic rhinitis: the patients perspective. J Allergy Clin Immunol 1997; 99:825-828
Mangosteen (Garcinia mangostana L.)
Available as a fruit extract supplement in juice or capsule form. Has xanthones, which have some antihistamine activity. Used as a Thai indigenous medicine for many years.
- Study results. Found that a 40% ethanol extract of mangosteen has potent inhibitory activities of both histamine release and prostaglandin E2 synthesis. Inhibitions of histamine release and prostaglandin E2 synthesis by mangosteen, a Thai medicinal plant. Biol Pharm Bull. 2002.
Butterbur (Petasites hybridus)
Available as an oral extract from this shrub has promise. Its major active compound appears to be petasin (a type of sesquiterpene ester). It has inhibitory activities on leukotriene generation in eosinophils and neutrophils. This indicates that it may have anti-inflammatory and anti-allergy properties (Even though butterbur does not seem to be effective in blocking histamine release). Butterbur also helps reduce smooth muscle spasm
- Buttebur extract found equally effective as non-sedative antihistamines. 6 randomized clinical trials studied butterbur extract used for AR and suggest that it is superior to placebo or similarly effective compared with non-sedative antihistamines for intermittent AR.
Herbal medicines for the treatment of allergic rhinitis: a systematic review.Ann Allergy Asthma Immunol. 2007. Department of Complementary Medicine, Peninsula Medical School, University of Exeter, England.
- Butterbur is an effective treatment for intermittent allergic rhinitis symptoms and is well tolerated for allergy relief. Found a study treating 186 patients for 2 weeks with butterbur or placebo.
Butterbur Ze339 for the treatment of intermittent allergic rhinitis: dose-dependent efficacy in a prospective, randomized, double-blind, placebo-controlled study. Arch Otolaryngol Head Neck Surg. 2004.
Spirulina
May help. Contains unusually high levels of fatty acid gamma-linolenic acid (GLA) (precursor to anti-inflammatory DGLA)
- Study demonstrated protective effect of a spirulina-based dietary supplement (Earthrise Nutritionals, Inc., Irvine, CA) towards allergic rhinitis -the study assessed the impact on the production of cytokines (Interleukin (IL)-4, interferon (IFN)-gamma, and IL-2) critical in regulating immunoglobulin E-mediated allergy. Results indicated that spirulina can modulate the Th profile in patients with allergic rhinitis by suppressing the differentiation of Th2 cells mediated, in part, by inhibiting the production of IL-4. J Med Food. 2005. Division of Rheumatology/Allergy and Clinical Immunology, University of California at Davis, School of Medicine, Davis, California, USA.
Stinging nettle herbal extract
May be helpful for allergic rhinitis. Typical dose is 300 mg/day of freeze-dried Urtica dioica.
NOT Grapeseed extract
Grapeseed extract found to be unhelpful in the treatment of fall seasonal allergic rhinitis.

Treatments for allergies aimed at the cause of inflammation
To see why we are dealing with chronic inflammation:
Causes of Chronic Low-Level Inflammation
For a comprehensive chart of tactical maneuvers to regulate inflammation in the body:
Treatments for long-term inflammation
Listed below are some of the “no-brainer” tactics and some successful, study-supported treatments specifically used against allergies.
Avoid allergens if possible
- Tobacco smoke /Strong chemical odors. Avoid these environmental irritants, which may increase sinus problems
- Pet dander. Move animals out of the general living space
- Dust mites – use impermeable mattress covers, wash bedding every week in hot water and remove all non-washable items from the bed (E.g. stuffed animals); remove bedroom carpets and upholstered furniture;
- Food. A food allergy reaction is not the same as food intolerance, which is instead, an undesirable effect (E.g. gas, nausea, diarrhea) of eating a particular food (maybe because they lack a necessary digestive enzyme). Foods containing allergens accounting for ~90% of food allergies, include wheat gluten, milk or other dairy products, soy, peanuts, nuts, fish, shellfish, or eggs. Taking stomach acid-reducing medications (E.g. Nexium®) may allow harmless food proteins to become potential allergens by limiting their digestion in the stomach.
- Cockroaches. Keep kitchen clean; put out traps.
- Pollen. Avoid communing with nature during the spring and early summer when grasses, trees, weeds (particularly ragweed) pollen usually occurs. Get someone else to mow the grass!
Consume Foods that control inflammatory reaction
Balance Omega-3 / Omega-6 intake
Reduce omega-6 intake. An increase in the use of margarine and vegetable oils containing inflammatory omega-6 polyunsaturated fatty acids has led to an imbalance with anti-inflammatory omega-3 fats. Omega-6 linoleic acid in such as corn/safflower/sunflower oils, is a precursor to arachidonic acid, which can be converted to prostaglandin E2 (PGE2) that causes the immune system to release a protein that triggers allergic reactions.
Increase anti-inflammatory Omega-3 DHA and EPA intake. Eat more cold water fish (E.g. salmon, herring, tuna, sardines) containing anti-inflammatory omega-3 fatty acids, which inhibit the formation of inflammatory prostaglandin PGE2. Since it is difficult to obtain sufficient omega-3 fat in today’s farmed fish, you should strongly consider supplementing with a marine oil, such as wild salmon oil.
- Supplement anti-inflammatory Omega-6 Di-homo-gamma-linolenic acid (DGLA). Metabolized from gamma-linolenic acid (GLA) found in high amounts in evening primrose, borage and blackcurrant oils, also inhibits the formation of inflammatory prostaglandin PGE2. With allergies, one should consider taking a GLA supplement, but not before dealing with likely omega-3 deficiency.
Borage, blackcurrant, or evening primrose oil for DGLA
Ensure sufficient intake of vitamin B6 (Pyridoxine),Magnesium, Zinc, vitamin B3 (Niacin) and vitamin C. Vitamin C is needed by the conversion enzymes D6D and D5D to provide pathways for production of anti-inflammatory prostaglandins and leukotrienes. E.g. If you don’t have enough D6D enzyme, you can’t ever make enough GLA (to convert to anti-inflammatory DGLA) from Omega-6 Linoleic Acid, which is contained in such as nuts, seeds and vegetable oils
EFAs -> Local Hormones – First Response Team
Magnesium regulates and suppresses histamine production. Histamine is released in response to various allergens, such as perfumes, pet dander, dust, pollen etc. – histamine causes allergy symptoms. An article in the prestigious British journal “The Lancet” reported that healthy magnesium levels are associated with lower rates of allergies and asthma. The best way to swiftly increase magnesium is via transdermal magnesium chloride or by nebulizing magnesium chloride
Ensure your body has a sufficiency of antioxidants. Through diet, via supplementation, or lifestyle choices
- Vitamins A, Vitamin C, Vitamin E, Coenzyme Q10;
- VITAMIN D. The best way to ensure you are getting enough of this powerful anti-inflammatory is to take a daily “sunbath”.
Vitamin D – The Sunshine Vitamin
- MELATONIN. Produced during a good night’s sleep in a darkened room, this hormone is a very powerful antioxidant that is generally overlooked.
MELATONIN -The Darkness Hormone
- Some good food choices for antioxidants –blueberries, pomegranates, cherries, grape seed, green tea, wine.
- Avoid trans fats, other damaged fats, and anything else that produces ROS in the body – depleting its precious antioxidant supply
Stress, Toxins, Damaged Fats, Microbes and NOT Enough Antioxidants
- Avoid excess alcohol consumption. May increase IgE levels and aggravate allergy symptoms.
Intestinal probiotics
Lack of intestinal microflora allows allergies, inflammatory conditions and autoimmune diseases to flourish. E.g. asthma, eczema;
Probiotic strain bifidobacterium longum relieves clinical symptoms of allergic rhinitis (hayfever)s













