Progesterone ( means "For Gestation") Supplementation - Aids conception / prevents miscarriage / maintains pregnancy in the common case of luteal phase deficiency (LPD)
"Get pregnant / Stay pregnant"

To better understand the role of the ovarian corpus luteum, see this short description of how an egg becomes a fetus “Journey of an Egg – From follicle to uterus“
What is luteal phase deficiency (LPD)?
LPD exists in some women whereby the ovarian corpus luteum is unable to produce sufficient PROGESTERONE necessary for conception and/or maintaining a nurturing environment for a fetus – necessary through the first 10 weeks of gestation (counted from day 1 of last period) until the placenta takes over production at considerably higher levels. Until then, to aid conception and/or prevent miscarriage, these women may need to supplement PROGESTERONE.
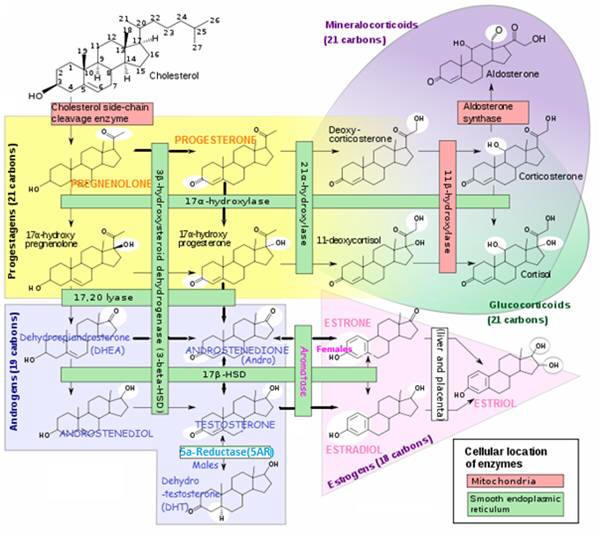
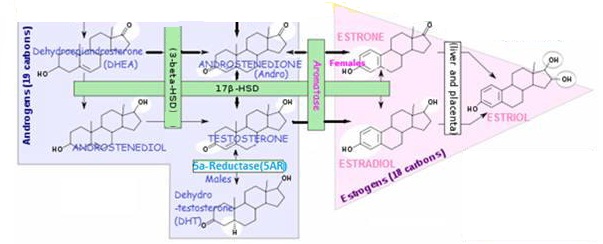
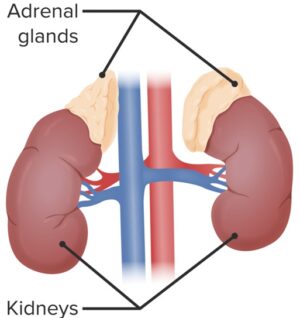
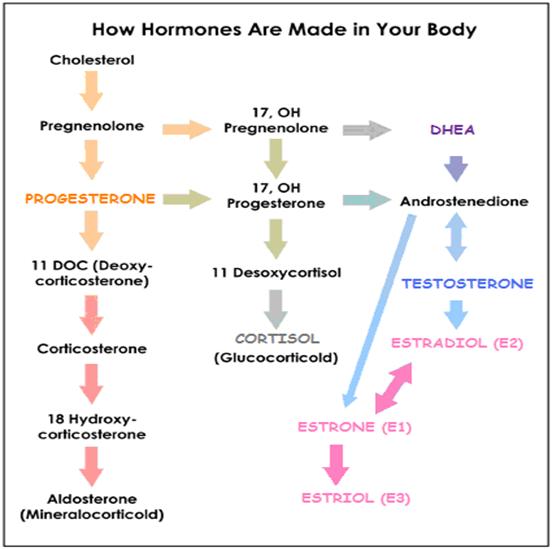
PROGESTERONE is a steroid hormone vital to the reproduction process. Produced by a corpus luteum in one of the two ovaries during the 2nd half of the menstrual cycle, by a process which breaks down cholesterol molecules. The ovaries take turns each month.
- During pregnancy, corpus luteum continues to produce PROGESTERONE until close to the end of the first trimester. At which time the placenta should have taken over production. Normal production of hormones, including PROGESTERONE, is significantly increased during pregnancy, especially by the third trimester.
Insufficient PROGESTERONE during pregnancy can result in:
- Uterine contractions. May cause miscarriage or premature labor
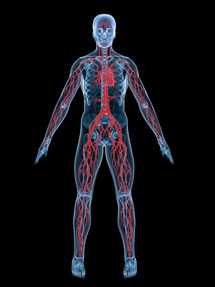
- Growth inhibition of new blood vessels. Needed to provide nourishment to the fetus.

What does progesterone do for conception and pregnancy?
PROGESTERONE production / availability is crucial for development of the fetus. A sufficiency of PROGESTERONE production by the ovarian granulosa cells of the corpus luteum in the early stages of pregnancy performs several necessary functions (which could be lacking with a luteal phase deficiency (LPD), where the corpus luteum is not producing sufficient PROGESTERONE):
- Stimulates growth of and maintains the uterine lining (endometrium). Where fertilized egg attaches itself; prevents premature shedding; thickens to a max. 4-6 mm
- Aids secretion of nutrients from endometrial (of uterine lining) glands. Maintains adequate blood circulation, stimulating growth of cells which feed the embryo
- Tempers immune system reaction to presence of “foreign body” 🙂
• Prevents mother’s immune system from responding to fetal antigens and rejecting the “new arrival”.• It does this by stimulating secretion of immune system Th2 and reducing secretion of Th1 cytokines.
• Overrides uterine contractions. Controls hypercontractility of smooth muscle cells in the middle layer of the uterine wall (myocytes);
- PROGESTERONE up-regulates HLA-G gene expression in first trimester trophoblasts. These cells are the first to differentiate from the fertilized egg, forming the outer layer of a blastocyst, which provides nutrients to the embryo and develops into a large part of the placenta. Evidence suggests that HLA-G also plays a critical role in maternal immune tolerance to the fetus;
- Prepares breasts for milk production
- Maintains proper function of the mother’s organs
- Controls blood pressure in later pregnancy. Higher serum concentrations of PROGESTERONE (but not ESTRADIOL) in early pregnancy were related to lower mean systolic blood pressures in the 2nd and 3rd trimesters;

Progesterone levels in pregnancy
Progesterone levels in early pregnancy ordinarily DOUBLES or TRIPLES during the first several weeks of pregnancy.
progesterone should be produced EVERY DAY during pregnancy (in the regular menstrual period, PROGESTERONE is only produced at ovulation and for about 14 more days).
- Normally when an egg is fertilized, chemical messengers cause the follicle to increase its production of PROGESTERONE to 30 to 40 mg per day. This is double or triple what it made during the luteal phase of the monthly cycle when the woman was not pregnant. The level of progesterone increases gradually until well into the third month of pregnancy. By that time, the placenta is well developed and is producing progressively more PROGESTERONE within the uterus.
- By the 3rd trimester progesterone levels rise to > 10-20 TIMES normal amounts. To protect the fetus, levels can be as much as 300mg to 400mg per day.
Signs / symptoms of low progesterone in early pregnancy
Low levels of progesterone during early pregnancy can result in the loss of the embryo. These are the signs to watch for:
- Spotting. The most common symptom of low levels of progesterone and human chorionic gonadotropin (hCG) hormone is bleeding in the first few weeks of gestation. While there can be other causes of this, any spotting that occurs, especially if it is accompanied by cramping, could be an indication of low levels of progesterone
- Tenderness in breasts / lower back. Although blood spotting is the most common indication of possible progesterone deficiency during early pregnancy, women who have been found to be deficient in progesterone during pregnancy have reported increased tenderness in the breasts and lower back pain combined with spotting within the first trimester. However, these symptoms by themselves may not be indicative of low levels of PROGESTERONE, and may be due to other things that are taking place in the body, such as the growth of milk-producing cells and fibrocystic swelling.

Progesterone supplementation can aid conception and prevent early miscarriage in women with a luteal phase deficiency (LPD)
PROGESTERONE therapy / supplementation provides a “tool” to aid conception and maintain a pregnancy in a woman with estrogen dominance or whose corpus luteum is not producing sufficient PROGESTERONE (termed luteal phase deficiency (LPD)). Either during the luteal phase of the menstrual cycle (latter half of cycle in humans) and/or after conception. Supplementing natural PROGESTERONE at the right time and dose can:
- Aid conception. Due to LPD, some women start bleeding before the 14 days after ovulation as the cause of failed conception. If this is the case, using PROGESTERONE at ovulation can help to lengthen the luteal phase. Using PROGESTERONE before ovulation could prevent ovulation occurring and therefore any chance of becoming pregnant. i.e. PROGESTERONE acts as a contraceptive before ovulation.
Significantly lower levels of PROGESTERONE are found in women with PCOS in the early luteal phase which may contribute to their delay in conception. LPD in PCOS may explain the anovulation and miscarriage that occurs in these women;
Prevent miscarriage during luteal phase of menstrual cycle and after conception. By countering estrogen presence after fertilization. Too much estrogen compared to PROGESTERONE during the luteal phase can cause miscarriage i.e. when follicles ovulate normally, but fail to continue their PROGESTERONE production at levels necessary for successful implantation of the fertilized egg and development of the embryo.
Maintain sufficient PROGESTERONE to maintain pregnancy until placenta takes over production. PROGESTERONE has many necessary roles in pregnancy – from controlling mother’s immune response (e.g. preventing untimely contractions) to providing nutrients for growing fetus. The placenta usually takes over the job of producing PROGESTERONE 10 weeks after gestation (which begins Day 1 of last period) – i.e. when fetus is 8 weeks old.
The effects of Estrogen during pregnancy are:
- Enlarges the uterus
- Enlarges genitals
- Stimulates the milk glands and enlarges breasts
- Increases blood volume by 30% and causes fluid retention;

Suggested progesterone dosage and regimen to promote and maintain pregnancy related to Luteal Phase Deficiency (LPD)
Risks of supplementing progesterone during pregnancy
Natural, bioidentical progesterone is generally safe to use during pregnancy – using up to 60-80 mg of bioidentical PROGESTERONE /day through the 10th week of gestation (i.e. 8th week after ovulation). Doses higher than 100 mg have some side effects, including sleepiness, loss of libido, mild depression, and hormonal imbalances.
progesterone supplementation may increase the risk of hypospadias – which is an abnormal placement of the opening at the end of the penis (can be corrected with surgery).
Prometrium ( a natural PROGESTERONE supplement) is categorized as a B drug for pregnancy by the FDA – which means there are no controlled studies finding it harmful in pregnancy. However, a 25-year study of > 2000 pregnancies found no increase in birth defects when using natural PROGESTERONE. (Pope Paul VI institute for the study of human reproduction)
Ensure your thyroid is producing enough thyroid hormones
Adequate levels of circulating thyroid hormones are important for normal reproductive function. These can be ensured by taking a daily dose of iodine.
What kind of progesterone to use and how to apply it?
Use only Bioidentical PROGESTERONE (concentrated at ~500mg PROGESTERONE / ounce) applied vaginally as first choice (or else topically)
- Synthetic forms (i.e. progestins) have too many health risks
- Oral doses are only 10% available after processing by liver
- Herbal PROGESTERONE, such as wild yam, is NOT recommended for this use
Long-term topical use (i.e. applied to skin) can cause a PROGESTERONE build-up in fatty tissues leading to excessively high blood PROGESTERONE levels – If you have been using topical PROGESTERONE long-term and maintain pregnancy, this is not a problem, since the pregnancy demands high levels of PROGESTERONE as it progresses into the second and third trimesters. However, if you miscarry, you could be dealing with untimely high levels of PROGESTERONE (as PROGESTERONE is slowly released from fatty tissues in the skin over several months), which would interfere with your natural menstrual cycles.
For information on different delivery routes and bioidentical PROGESTERONE:
Dellivery routes choices for supplementing PROGESTERONE
Doses of progesterone before and after conception
Dose BEFORE becoming pregnant? – 1/8 tsp (10mg) A.M. and P.M. (a total of 20mg /day) to correct luteal phase deficiency and enable pregnancy in cases where the follicle is still able to “pop” an egg.
- Begin supplementation the day after ovulation FOR 14 DAYS then stop. To figure PROGESTERONE start date, count back 14 days from when your next period is due (Day 1). Alternatively, use a fertility monitor to accurately ascertain when you ovulate.
As soon as pregnancy is confirmed, a woman at risk for miscarriage should start using natural USP PROGESTERONE (in cream or vaginal suppositories)
- Gradually increase supplemental PROGESTERONE dose from 20 mg up to 60 mg (or if necessary, even 80 mg) PER DAY.
- Whatever dose you are on, it should be split into at least 3 applications to more closely emulate the natural PROGESTERONE production from the ovarian corpus luteum– PROGESTERONE lasts about 7 hours in the system.
Do not miss a dose by forgetting or running out of supplies – YOU COULD MISCARRY
- Keep supplemental PROGESTERONE with you at all times and apply 20 mg PROGESTERONE immediately if you experience any cramping, in an effort to stave off a miscarriage.
You must continue taking PROGESTERONE for at least 8 weeks after ovulation i.e. 10 weeks’ gestation – at which time the placenta should be producing enough PROGESTERONE to maintain the pregnancy. During the last trimester, PROGESTERONE production in the placenta increases to a level that supplemental PROGESTERONE becomes superfluous.
Resume one month after delivery to prevent post-partum depression – at 20 mg per day. Natural PROGESTERONE is useful for post-partum depression, which many women experience after childbirth. Serum allopregnanolone levels are significantly lower in women experiencing postpartum “blues” -allopregnanolone is a metabolite of PROGESTERONE; multiple studies confirmed that PROGESTERONE supplementation via IUD’s did not adversely affect breast-feeding.

References
Online article by John R. Lee, M.D. and Virginia Hopkins, BEATING INFERTILITY – Getting Pregnant and Staying Pregnant. Link














![<span class="ACETYLCHOLINE">Acetylcholine (Ach)</span><span class="hdg-smaller"> – Movement, memory, learning neurotransmitter</span> – [Cloned #60543]](https://healthhappening.com/wp-content/uploads/2025/12/Ach.jpg)