How to supplement PROGESTERONE to counter estrogen dominance


Use PROGESTERONE supplementation cautiously
*** FIRST***- Please read: Estrogen dominance treatment 1-2-3
PROGESTERONE supplementation therapy used to counter estrogen dominance is the last-resort step of a 3-step treatment . FIRST, use other tactics to NATURALLY reduce estrogen levels in the body and boost PROGESTERONE via diet and lifestyle changes before considering supplementation. For example:
- Ensure liver’s efficient removal of estrogen metabolites from the body. A retention coffee enema is most effective to cleanse the liver – very effective for stimulating bile production in the liver
- Ensure sufficiency of Magnesium and vitamin B6 – required to remove estrogen metabolites from the body
- Reduce exposure to environmental xenoestrogens and do not consume excess phytoestrogens
An estrogen-dominant body tries to compensate by desensitizing its estrogen receptors, making them less sensitive to estrogen. However, because natural PROGESTERONE re-sensitizes the estrogen receptors to normal sensitivity, if one uses natural PROGESTERONE without first getting rid of exposure to xenoestrogens / excess phytoestrogens symptoms would likely get worse (E.g. cysts get bigger, breasts become sorer, more bloating and fat gain around the middle).
Be patient – After cutting out xenoestrogens and excess phytoestrogens, it takes about 1-3 months, for these “undesirables” to leave the body.
Xenoestrogens – “Endocrine Disruptors”
Used in the long-term, it is important to use a delivery route that avoids hormonal build-up in the fat cells. This problem is now recognized as a consequence of long-term transdermal application.
An annual urine test (most accurate) or saliva test (next best alternative) to monitor PROGESTERONE levels is advisable. The saliva value should be below 300 (some have reported numbers over 10,000, which may take up to two years to return to normal, since PROGESTERONE is stored in the fat and releases very slowly). If PROGESTERONE level is not below 300, one should not resume PROGESTERONE until it is.
To understand why blood tests for hormones are useless:
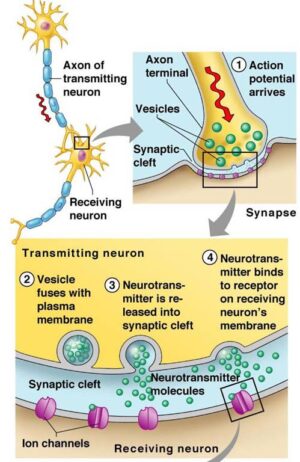
PROGESTERONE supplementation may INITIALLY have an estrogenic effect. PROGESTERONE reactivates “sleepy” estrogen receptors. In premenopausal women, a deficiency of PROGESTERONE causes a “turning-down” of estrogen receptor sensitivity, and when women begin using PROGESTERONE , those Estrogen receptors are reactivated. This causes them to become overly sensitive, with ensuing estrogen dominance effects – e.g. water retention, headaches and swollen breasts. There can also be a temporary buildup of the endometrium, causing spotting and irregular bleeding. Most of these symptoms should disappear within a couple of cycles.

Use only bioidentical PROGESTERONE
Any PROGESTERONE supplementation therapy should use BIOIDENTICAL PROGESTERONE. i.e. the identical molecule that your body produces.
The label should say U.S.P. PROGESTERONE . USP (United States Pharmacopeia) means the formulated PROGESTERONE is of pharmaceutical grade and provides assurance that the product is bioidentical to that which is secreted from the female ovaries.
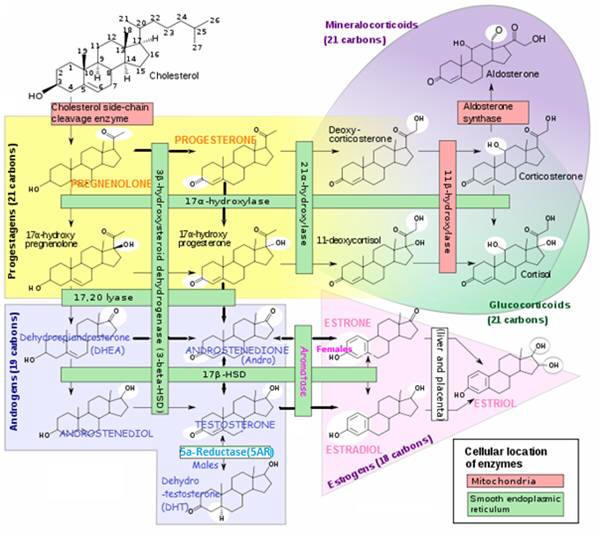
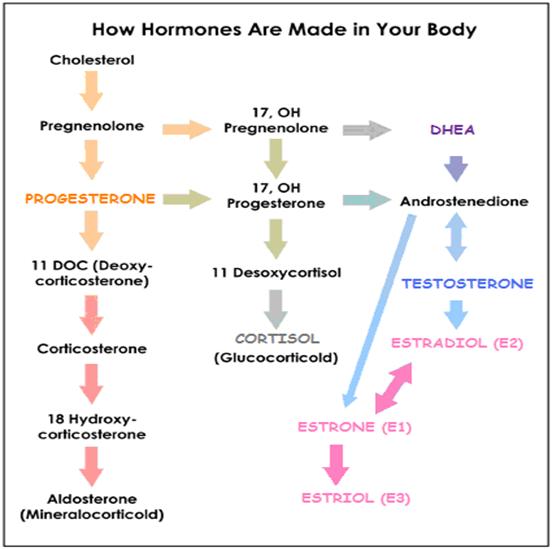
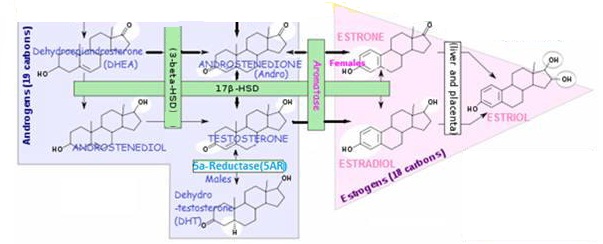
Natural, bioidentical PROGESTERONE is NOT DIRECTLY found in any plant. It is synthesized from fat saponins such as diosgenin from Mexican wild yam or soy. After extraction from a plant source it is chemically modified / compounded in a laboratory -since the body can not metabolize diosgenin (derived from plant dioscin) into PROGESTERONE. Until 1970, wild yam was the main base source for production of PROGESTERONE in the contraceptive pill, and as a precursor for corticosteroids, such as CORTISONE. Today, natural and bio-identical PROGESTERONE is mostly produced from soybeans.
- “Natural” does not necessarily mean “bioidentical”. Bioidentical term refers to the shape of the molecule rather than the source of the hormone being identical. Some formulations may have been derived from plant-based sources, but are not even close to the shape of the natural molecule. E,g, Numerous plant-based HRT and purely yam-based creams that have not been chemically-modified.
- Soybean-source PROGESTERONE should use a NON-GMO soy
Cream / Gel should contain 1.5-3% USP natural PROGESTERONE by volume – this is equivalent to 450-900 mg /oz. of cream. When used transdermally, PROGESTERONE is absorbed into the fat and is released from the fat into the blood stream in direct proportion to the concentration of the cream. A higher dose cream will not release the hormone into the blood stream smoothly over a 12 hour period, and since PROGESTERONE only has a half life of five minutes once it is in the blood, this will significantly limit its effectiveness.
The de facto standard cream concentration is 500 mg of PROGESTERONE in 30g of cream (1.6%)
~¼ tsp. contains ~20mg
PROGESTERONE cream / gel / suppositories should NOT contain parabens as preservatives. They should also be free of any other harmful substances. E.g. liquid paraffin, parabens, phenoxyethanol, sodium lauryl sulphate, propylene glycol, fragrances, artificial colours and PEG emulsifying waxes (can contain the carcinogen dioxane).
Bioidentical PROGESTERONE cream products include:
- Imagine Dermatology Prog-Relief;
- NOW® Natural PROGESTERONE (wild yam, 1.54%);
- Natpro (Non-GMO soy). Contains the maximum allowed dosage of USP PROGESTERONE from soy (3.33%) – Use smaller amount, quicker to rub in and absorb than weaker creams
- Emerita Life-flo Pro-gest® (wild yam);
Bioidentical oral PROGESTERONE includes:
- Prometrium
Do NOT Use Synthetic PROGESTERONE (a progestin) – different to bioidentical PROGESTERONE produced by the body
Crinone® Vaginal Gel and oral progestins, such as Provera®, Premarin®, Prempro® and Megestrol®, are patented synthetic hormones. They are NOT the same as the PROGESTERONE produced by the body. However, they do compete with the receptor / binding sites normally reserved for natural PROGESTERONE. By chemically altering the natural PROGESTERONE, drug industries are able to file patents and make multi-billion-dollar profits.
- Progestins have different effects. Some will activate the receptor in a manner similar to the natural hormone, some will have a greater effect, others will have no effect or will block the receptor completely.
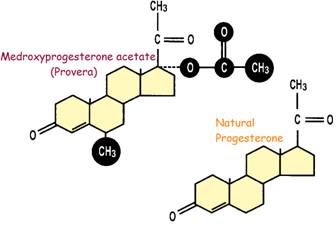
PROGESTERONE – Synthetic vs Natural Molecules
Progestins are potentially highly toxic because of their altered molecular structure. In the body, progestins undergo different chemical reactions than natural PROGESTERONE , which causes several serious, unpleasant side effects and health risks not associated with natural PROGESTERONE, such as:
- Breast cancer
- Strokes
- Fluid retention
- Migraine headaches
- Asthma
- Cardiac irregularities (can destroy estrogen’s beneficial effects of maintaining or raising HDL levels)
- Mood disturbances (E.g. depression)
- Birth defects.
Synthetic sex hormones – Frankenstein versions of natural hormones
Women with a history of hypertension, diabetes, weight problems, varicose veins, atherosclerosis, breast or uterine cancer, and recurrent UTIs and vaginal infections should definitely NOT take a progestin (or a synthetic estrogen, such as ethinylestradiol, a conjugated equine estrogen (CEE), such as Premarin® or Duavee®, or a synthetic CEE, such as Cenestin® or Enjuvia® ). Since it will likely exacerbate those conditions.

How much PROGESTERONE to use, when to use it, and for how long?
How long to supplement?
A minimum 2-3 months supplementation – needed to raise and maintain your PROGESTERONE level for maximum improvement of symptoms due to estrogen dominance. For menopause and osteoporosis treatment, use PROGESTERONE cream indefinitely.
How much USP bioidentical PROGESTERONE should you use and when?
Proper dosage and compliance are essential
The right dose is the dose that works, but . . . – when it comes to balancing hormones, more is not better. The amount required depends on the specific application and should be tailored to the individual’s needs and response. To avoid hormonal imbalance one should not use higher than the recommended dosage; A dosage chart is given as a guideline (most dosages recommended by Dr. John R. Lee, MD for transdermal application):
FDA-approved ORAL Dose. In Oct 1999, the FDA approved a 200 mg daily dose of Prometrium, an oral PROGESTERONE , for use in preventing uterine cancer in women taking estrogen– i.e. this dose has been acknowledged as sufficient to oppose estrogen. Bear in mind that a 200 mg dose of oral PROGESTERONE actually delivers about 20 mg of PROGESTERONE (also be aware that with oral administration, 180 mg is excreted by the liver or transformed into other substances, which can cause problems).
The cream, gel or suppositories are best used twice a day – to better simulate the body’s natural production. With slow-release bio-adhesive gel, once/day may be sufficient (follow package instructions)
Pre-menopausal women
Pre-menopausal women must take at least 3-7 days off each month without applying any PROGESTERONE cream / gel / suppository – since the body’s natural production of PROGESTERONE is cyclical, supplementation should ideally mimic the body’s naturally changing concentrations to affect a proper physiological response. i.e. the body should recognize some times when the PROGESTERONE level is low.
- Non-ovulating – PROGESTERONE supplementation should re-create what your body would produce if you were ovulating – both in the timing and amount used. The usual dose is 15-24 mg/day for 14 days before expected menses, stopping the day or so before menses.To figure the PROGESTERONE start date, count back 14 days from when your next period is due (i.e. Day 1 of next cycle), then beginning on that date, supplement PROGESTERONE for 14 days. The abrupt lowering of the PROGESTERONE level is the primary trigger for starting your period, at which time any PMS and painful periods will be dramatically reduced.
- Ovulating – wait until the day after ovulation (i.e. the luteal phase) to begin supplementation, which will then augment the body’s own PROGESTERONE production from the corpus luteum. Supplementation should continue through the last 14 days of the cycle. After which, stopping the supplementation should initiate menses. Using PROGESTERONE earlier than ovulation would prevent ovulation resulting in no corpus luteum and therefore no PROGESTERONE production, which would be working against the body’s own mechanisms. To accurately determine ovulation, you should purchase a fertility monitor.
Menopausal women – may only need ~15 mg PROGESTERONE, but taken for the first 25 days of the month, then take 5 or 6 days off without applying any PROGESTERONE cream/gel/suppositories – so that one’s body will not develop resistance or tolerance to the PROGESTERONE , and so become ineffective. Restart on the first of the month.
Men – may need 5-10 mg / day to keep in range of their normal, low, but constant amounts of PROGESTERONE production and counter estrogenic presence. Take 5 or 6 days off each month without using any PROGESTERONE cream/suppositories so that one’s body will not develop resistance or tolerance to the PROGESTERONE .

Ensure sufficiency of magnesium and B-vitamins
It is essential to ensure sufficient B-vitamins and Magnesium whilst supplementing PROGESTERONE.
Magnesium & B vitamins aid liver’s estrogen clearance
- B-vitamins. You need ~5-8 mg of B6 along with all the other B-complex vitamins.
- Magnesium – The Missing MIneral. Supplement with 400-600 mg oral magnesium and also use transdermal magnesium for a few months to quickly increase magnesium levels in your body.

Delivery route choices for supplemental PROGESTERONE
PROGESTERONE supplementation should try to emulate the body’s natural production
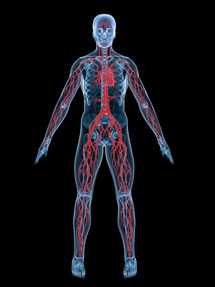
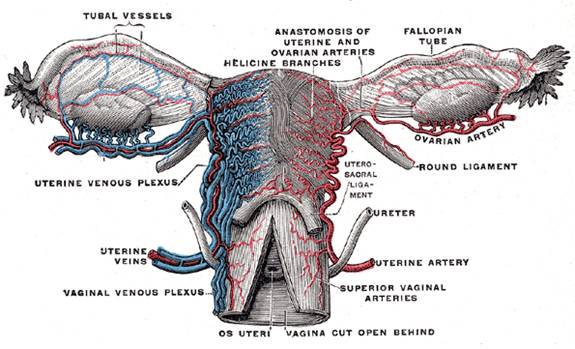
PROGESTERONE is produced naturally by the ovaries and adrenals – for transport into the blood stream and delivery to hormone-sensitive cells in the body. PROGESTERONE is produced by the ovarian corpus luteum during the luteal phase (following ovulation) of the menstrual cycle Ovarian connections are located in the pelvic area:- The fallopian tubes directly connect the ovaries to the uterus.
- The ovaries empty into a pelvic plexus of veins having direct access to the blood stream – Substances absorbed through the vaginal membranes also enter this same pelvic plexus of veins.
- The vaginal route is best for women
- The scrotal (possibly with permeation enhancement, such as combining with DMSO) or rectal routes are best for men
The delivery route choices

Oral delivery route for progesterone
NOT a good choice for any steroid hormones
80-90% of oral PROGESTERONE is destroyed in GI tract and liver (so-called “first pass”liver metabolism). Even when micronized and in oil, or with fatty foods (it does not dissolve in water). PROGESTERONE does not have any natural reason to be in the GI tract, which is not an efficient transport route for any steroid hormone. Swallowed hormones encounter absorbing foods, but PROGESTERONE is not affected by stomach acid. “Survivors”must later be broken down by the liver, and since only 10-20% reaches target cells a dose 5 times higher than utilized is needed.. Simon JA et al, 1993
When processing PROGESTERONE , the liver creates >30 different metabolites. These can have several undesirable side-effects. Notably 5a-reduced metabolites are known to cause neuropsychological side effects. Arafat et al addressed the sedative and hypnotic effects that may be mediated through these metabolites. The bioidentical PROGESTERONE Prometrium® can have several unpleasant side-effects. Kalil Nahoul et al, 1993; Arafat ES, 1988

Topical / Epithelial delivery route for PROGESTERONE (i.e. via skin using hormonal cream/gel)
NOT for LONG-TERM USE – with prolonged use, PROGESTERONE can build up in fatty tissues, where its constant release can result in an overdose
Using topical PROGESTERONE for systemic supplementation
- Delivered transdermally, PROGESTERONE enters the blood stream fully bio-available (i.e. not bound to protein in serum). PROGESTERONE is absorbed through the epithelial tissue of the skin and into the bloodstream without passing through the liver. The increase in PROGESTERONE is very apparent in saliva testing (a serum test will show little or no change, since blood tests do not accurately reflect body’s PROGESTERONE status. See: Testing for Hormones);
- Dermal fatigue from long-term skin application. Used in the short-term, the transdermal method has been employed for the past several years with much success. HOWEVER, a problem, identified as “dermal fatigue”, has become apparent with its long-term use . Being fat-soluble, fat cells in the skin store the hormone, which is fine at first, since fat stores are low. Unfortunately, after a few weeks of applying cream to skin, the skin tissue fat cells become saturated with PROGESTERONE (or any other steroid hormone used), which results in disruptions to adrenal hormones, such as DHEA, CORTISOL and TESTOSTERONE. This not only stops the effectiveness of the hormone, it may even make symptoms worse.
- Users of transdermal PROGESTERONE cream long-term can have excessively elevated levels of this hormone. Those with excessively high PROGESTERONE levels from using transdermal supplementation may need to go off the cream for up to two years, to allow the excess PROGESTERONE to leave their body.
Some topical PROGESTERONE applications for the benefit of the skin itself
- Good on piles or painful, achy or itchy areas.
- Excellent for burns
- Anti-aging on the face.
- The cream can also be applied in the vagina or nose to counter dryness.
How often should you apply topical PROGESTERONE
- Take at least three to seven days off every month – 3 days for those women who experience a severe recurrence of symptoms during the break; taking a break prevents one’s body from developing a resistance or tolerance to the PROGESTERONE .
- Transdermal PROGESTERONE cream is better applied in split doses. To keep levels consistent; Divide into at least two doses if you are using a high dose of PROGESTERONE (40mg or more) – E.g. 2/3 at bed time and 1/3 in AM.
Application areas
- Neck, face, arms, chest, legs, stomach, vagina, scrotum
- Scrotal Route (for delivery to the prostate gland in men).
Special note for scrotal application (a good application area when used against prostate cancer for delivery to the prostate gland). Simply rubbing the PROGESTERONE cream into the scrotal area may allow sufficient absorption of PROGESTERONE – however, this author suggests using a small amount of the membrane penetrant DMSO to carry the PROGESTERONE cream through the scrotal membrane to enhance absorption, DMSO must be applied on clean, dry skin with clean hands. Application area must be allowed to dry completely after application before being allowed to touch other material.
Do not attempt to use DMSO without first getting to know how to use and handle it:
DMSO – Medicine Carrier / Cell membrane
- Alternatively, a World Intellectual Property Organization patent (WO2005079317) describes the successful absorption of PROGESTERONE through the scrotal membranes using certain substances (polyethylene glycols or peptide/fatty acid complexes) to enhance absorption
“Permeation rate enhancers allow for rapid absorption of the PROGESTERONE composition across the scrotal sac, after which the lipophilic PROGESTERONE hormone is stored in adipose cells. After the PROGESTERONE hormone reaches a saturation level in the adipose cells, it diffuses into the circulatory system for eventual uptake by the prostate gland. The present invention therefore can deliver a sustained effective dosage amount of PROGESTERONE to the prostate gland.”
Rub the PROGESTERON cream into the skin
- Skin comprises 95% kerotinocytes with many PROGESTERONE receptor sites.
- The skin must be clean. Cleared of cosmetics etc. cream is better absorbed when applied immediately after drying off after bath or shower;
- Rotate among three or four different skin sites on different days. The larger the area of skin the dose is spread on, the greater the absorption; areas typically used are neck, chest, inner arms, inner thighs, and stomach

Rectal delivery route for PROGESTERONE (Using hormonal cream/gel)
Epithelial tissue forms the covering or lining of all internal and external body surfaces
Rectal delivery of PROGESTERONE using suppositories / pessaries is the PREFERRED supplementation choice for men
- Avoids hormonal build-up in fat cells. This improvement to PROGESTERONE delivery method avoids the hormonal build-up in fat cells that occurs with the transdermal method. Dr. Jonothon Wright, another pioneer in bio-identical hormone supplementation (in addition to the now deceased Dr. John Lee), uses this method in his clinics.
- The rectum has a mucosal epithelial surface similar to the vagina. Chakmakjian et al found that RECTAL administration of micronized PROGESTERONE in normally menstruating women (during the follicular phase) yielded increased under-the-curve areas of serum PROGESTERONE compared to doses of sublingual, oral or vaginal micronized PROGESTERONE . Chakmakjian ZH, 1987
- Suppositories / Pessaries may make rectal application of the hormone a little easier, but it does make it messier. PROGESTERONE is usually combined with a highly saturated fat, such as cocoa butter. This will harden at cooler temperatures, but melt at body temperature.
Rectal PROGESTERONEadministration has a wide range of absorbability
- Blood drainage from the lower end of the rectum is directly into systemic circulation via the vena cava. Drainage is via both venous blood capillaries and lymphatic vessels. When an active component is absorbed in the lower portion of the rectum (via the inferior hemorrhoidal veins) it reaches the general circulation directly – bypassing the hepatic first-pass elimination. Ritschel WA, 1991
- However, if the compounds are absorbed by the upper part of the rectum (superior rectal ampulla) they will reach the portal circulation (via the superior hemorrhoidal vein). Thus the liver gets the “first pass” at the PROGESTERONE with the inherent problems seen in oral administration. de Boer AG et al, 1982
Drawbacks of rectal administration
- Defecation affecting absorption;
- Lack of patient acceptability.

Vaginal delivery route for PROGESTERONE (Using hormonal cream / gel)
Epithelial tissue forms the covering or lining of all internal and external body surfaces
Vaginal delivery of PROGESTERONE is the preferred supplementation choice for women
- Particularly when uterine effects need to be maximized or blood concentrations minimized to limit side effects. PROGESTERONE as gel, suppositories or cream is applied to the mucous epithelial membrane lining the vagina. This delivery method avoids “first-pass” liver metabolism problems of oral delivery.
- Avoids hormonal build-up in fat cells. This improvement to PROGESTERONE delivery method avoids the hormonal build-up in fat cells that occurs with the transdermal method. Dr. Jonothon Wright, another pioneer in bioidentical hormone supplementation (in addition to the now deceased Dr. John Lee), uses this method in his clinics.
Vaginal application PROGESTERONE choices
- PROGESTERONE cream rubbed directly on vaginal epithelial membranes. Using finger-tips it is possible to reach pretty far into the vagina.
- Bio-adhesive gel preparations. These preparations cling to the vaginal membrane, and thus work better than cream formulations and suppositories, which can cause inconvenient vaginal discharges and possibly an irregular absorption of the active component. Sustained release (Gel) forms of PROGESTERONE, alleviate the need for multiple daily treatments.
- Vaginal suppositories / Pessaries. If you cannot find these or they are not cost effective, you could make your own by mixing required dose with cocoa butter, which hardens at room temperature, but melts at body temperature. You will need to find some little bullet-shaped molds or use some other ingenious method to shape the suppositories. If only used once per day, it is best used at night (when you are lying down) to prevent gravity-leakage.
Vaginal route mimics ovarian PROGESTERONE delivery into blood stream. Ideally, a woman wants to mimic the way pre-menstrual ovaries get hormones directly into the blood stream.
- The ovaries are in the pelvis, and have direct access to the blood stream via a pelvic plexus of veins
- Hormones absorbed through the vaginal membranes also enter the same pelvic plexus of veins emptied into by the ovaries. Hormones are then transported to the heart and lungs and distributed to your tissues just as if your ovary had actually produced them.
Vaginal application closely mimics the body’s own hormonal delivery system
There seems to be a preferential distribution of PROGESTERONE to the uterus following vaginal administration
- Studies strongly suggest a direct local “portal” for vagina-to-uterus transport of PROGESTERONE . This phenomenon was found to involve the vascular system and confirmed the existence of the so-called “first uterine pass effect”. Cicinelli E et al, 1998
- The lymphatic system of the upper part of the vagina, being in direct communication with the lymph vessels of the uterus may also represent a potential route for direct passage to the uterus of substances applied to the vagina. Transvaginal PROGESTERONE ,1999
Vaginal PROGESTERONE administration results in a high concentration at the local uterine / endometrial level – despite generally lower plasma levels than transdermal or intergluteal routes
- “First Uterine Pass Effect”. The vaginal route is a better choice if the uterus / endometrium is the target area – PROGESTERONE has a direct impact on the uterus before entering circulation (the so-called first uterine pass effect). Von Eye et al, 2004; Alam V et al, 2001; Weckstein LN et al, 1993; Maddocks S et al, 1986; de Ziegler D, 1995;
- Studies showing that vaginal PROGESTERONE resulted in low serum levels, but efficacious endometrial concentrations. Since PROGESTERONE is absorbed locally, it does not permit high plasma levels of PROGESTERONE , it therefore has less undesirable systemic effects.
– Vaginal gel dose used in the luteal phase at 45mg every 48 hours resulted in low serum PROGESTERONE but endometrial efficacy was unhampered. also, serum PROGESTERONE does not predict effects of vaginal PROGESTERONE on endometrium; Fanchin R et al, 1997
– Miles and coworkers also demonstrated that vaginal administration led to lower serum and higher endometrium PROGESTERONE concentrations compared to measurements after I.M. delivery. Miles RA, 1994
– Gibbons and coworkers compared vaginal and intramuscular (I.M.) PROGESTERONE delivery in women undergoing egg-donor programs, with higher mean serum PROGESTERONE in I.M. group. All subjects in both groups had an endometrial histology that was “in phase” (meaning the 4 phases, menstrual, proliferative, secretory, and pre-menstrual, of the menstrual cycle were on schedule) Vaginal PROGESTERONE delivery has been shown as effective as intramuscular injections for raising endometrial levels and maintaining pregnancy. Gibbons WE et al, 1998
Vaginal PROGESTERONE absorption may be influenced by the degree of vaginal mucosa estrogen content after estrogen treatment. Villanueva et al, 1981
Vaginal PROGESTERONE absorption may be influenced by the type of the formulation used:
- Different bases of suppositories. Tests on glycerinated gelatin, cocoa butter and polyethylene glycol found that they all raised levels above baseline for the same duration, but polyethylene glycol raised the mean peak level of circulating PROGESTERONE the highest. Price et al, 1983
- PROGESTERONE particle size. Micronized PROGESTERONE in non-liquefying cream showed promise for a goal of a single daily application. Kimzey et al, 1991
Vaginal PROGESTERONE delivery has been successful for HRT for various conditions Warren et al 1999, including menopause de Zeigler et al, 1999
High PROGESTERONE concentration at uterine level has advantages when supplementing PROGESTERONE for luteal phase support
- For pregnancy or HRT. Which has the goal of inducing adequate endometrial secretory transformation. Before ovulation, PROGESTERONE levels in a woman’s body remain relatively low, but rise after ovulation during the latter part of a woman’s menstrual cycle which is called the luteal phase. The luteal phase begins with the production of PROGESTERONE and ends with either pregnancy or menstruation, when the uterus sheds its lining. During pregnancy, PROGESTERONE helps to maintain the lining of the uterus, providing necessary nutrients to support and nurture a fertilized egg.
- For pregnancy, the dose amount and timing is crucial. This is because PROGESTERONE may (i) Act in favor of implantation as a permissive factor in a certain range of concentration or (ii) Block implantation when its concentrations are lower or higher than cut-off values. Villanueva B et al, 1981; Erny R et al, 1989
E.g. Some of the first contraceptives used a high dose of PROGESTERONE. The timing of the dose should lend support to the natural luteal phase. Penzias et al used Crinone 8%, a vaginal gel containing 90 mg micronized PROGESTERONE in a polycarbophil base, to support luteal phase to support pregnancy after IVF, with rates comparable to intramuscular administration or vaginal suppositories. Penzias AS, Alpcr MM, 2003; Anserini P et al, 2001; Lightman et al, 1999
- Vaginal PROGESTERONE Is equally effective In achieving pregnancy outcomes as injectable PROGESTERONE In donor egg cycles. 105 recipients at Boston IVF treated with vaginal PROGESTERONE achieved a 58.1% pregnancy rate and a 51.4% delivery rate, versus a 53.3% pregnancy rate (p=0.503) and a 48.3% delivery rate (p=0.689) for patients receiving intragluteal PROGESTERONE Med News Today, 16 Apr 2008
- Commonly used in many countries for luteal support in reproduction-assisted therapies. E.g. for IVF (In vitro fertilization) Bourgain C, et al, 1990; Artini PG et al, 1995

Sublingual route for progesterone
Drops of PROGESTERONE in an oil-based suspension are placed under the tongue. Enter the blood stream directly and will not build up in your tissues like dermally applied cream. This method is preferred by Dr. Raymond Peat because it is efficiently absorbed through mucosa in the mouth. Sublingual PROGESTERONE , being fat-soluble is more effective when dissolved in vitamin E. He purports that it will stimulate the ovaries to produce PROGESTERONE (if the ovaries are still functioning) and will energize the adrenals and thyroid. Since each drop is about one milligram, you can determine an accurate dose. However, IT IS VERY BITTER!
- Sublingual PROGESTERONE for hot flashes, migraines and cramping (at 15 minute intervals until symptoms resolve) has been suggested.

Intramuscular (I.M.) Injection route for progesterone
Most common administration in clinics. Injections cause pain at injection site, are inconvenient and invasive;
Get the hormone directly into the blood stream – and are tolerated by those women highly motivated to reduce threat of abortion, prevent pre-term labor and for assisted reproduction (especially those with PCOS who are resistant to clomiphene citrate, which is used to stimulate hormones promoting ovulation); for those not willing to undergo the pain, this is not an effective method for long-term treatments.
Guarantees adequate and verifiable plasma levels of active component.
Effective in infertility.
PROGESTERONE half-life significantly longer than when injected into arm. Due to higher concentration of adipose cells, which store then release PROGESTERONE wwhen plasma levels decrease;

References
Alam V, Vega M, Risquez F. Luteal phase support. Reprod Biomed Online 2001;3:250-262.
Anserini P, Costa M, Remorgida V, Sarli R, Guglielminetti E, Ragni N. Luteal phase support in assisted reproductive cycles using cither vaginal (Crinonc 8) or intramuscular (Prontogcst) PROGESTERONE : results of a prospective randomized study. Minerva Ginecol 2001;53:297-301. PubMed
Arafat ES, Hargrove JT, Maxson WS, Desiderio DM, Wentz AC, Andersen RN.Sedative and hypnotic effects of oral administration of micronized PROGESTERONE may be mediated through its metabolites. Am J Obstet Gynecol. 1988 Nov;159(5):1203-9. PubMed
Artini PG, Volpe A, Angioni S, Galassi MC, Battaglia C, Genazzani AR. A comparative, randomized study of three different PROGESTERONE support of the luteal phase following IVF/ET program. J Endocrinol Invest. 1995 Jan;18(1):51-6. PubMed
Bourgain C, Devroey P, Van Waesberghe L, Smitz J, Van Steirteghem AC, Effects of natural PROGESTERONE on the morphology of the endometrium in patients with primary ovarian failure. Hum Reprod. 1990 Jul;5(5):537-43. PubMed
Can KJ. ABC of endocrinology. I. Hormones in general. Lancet 1970; 1:763-765.
Chakmakjian ZH, ZachariahNY. Bioavailability of PROGESTERONE with different modes of administration. J Reprod Med 1987;32:443- 448. PubMed
Cicinelli E, Cignarelli M, Sabatelli S, Romano F, Schonauer LM, Padovano R, Einer-Jensen N. Plasma concentrations of PROGESTERONE are higher in the uterine artery than in the radial artery after vaginal administration of micronized PROGESTERONE in an oil-based solution to postmenopausal women. Fertil Steril. 1998 Mar;69(3):471-3. PubMed
de Boer AG, Moolcnaar F, de Lecdc LG, Breimcr DD. Rectal drug administration: clinical pharmacokinetic considerations. Clin Pharmacokinct 1982;7:285-311. PubMed
de Ziegler D. Hormonal control of endometrial receptivity. Hum Reprod. 1995 Jan;10(1):4-7.
Erny R, Simoncini C, Chastclliere N, de Lignres B. Variation de la PROGESTERONE plasmatiquc induites par l’administration vaginale d’Utrogcstan. J Gynecol Biol Reprod 1989; 18:229-234.
Fanchin R, De Ziegler D, Bergeron C, Righini C, Torrisi C, Frydman R. Transvaginal administration of PROGESTERONE . Obstet Gynecol. 1997 Sep;90(3):396-401. PubMed
Gibbons WE, Toner JP, Hamacher P, Kolm P. Experience with a novel vaginal PROGESTERONE preparation in a donor oocyte program.Fertil Steril. 1998 Jan;69(1):96-101. PubMed
Kimzey LMKimzey LM, Gumowski J, Merriam GR, Grimes GJ Jr, Nelson LM. Absorption of micronized PROGESTERONE from a nonliquefying vaginal cream. Fertil Steril. 1991 Nov;56(5):995-6.PubMed
Khalil Nahoul, Louis Dehennin, Michel Jondet, Marc Roger. Profiles of plasma estrogens, PROGESTERONE and their metabolites after oral or vaginal administration of ESTRADIOL or PROGESTERONE. Volume 16, Issue 3, Pages 185-202, May 1993 Maturitas
Lightman A, KoI S, Itskovitz-Eldor J. A prospective randomized study comparing intramuscular with intravaginal natural PROGESTERONE in programmed thaw cycles. Hum Reprod 1999; 14:2596- 2599. PubMed
Maddocks S, Hahn P, Moller F, Reid RL. A double-blind placebo- controlled trial of PROGESTERONE vaginal suppositories in the treatment of premenstrual syndrome. Am J Obstet Gynecol 1986;154:573- 581.
Miles RA, Paulson RJ, Lobo RA, Press MF, Dahmoush L, Sauer MV. Pharmacokinetics and endometrial tissue levels of PROGESTERONE after administration by intramuscular and vaginal routes: a comparative study. Fertil Steril. 1994 Sep;62(3):485-90. PubMed
Penzias AS, Alpcr MM. Luteal support with vaginal micronized PROGESTERONE gel in assisted reproduction. Reprod Biomed Online 2003;6:287-295. PPubMed
Price JH, Ismail H, Gorwill RH, Sarda IR.Effect of the suppository base on PROGESTERONE delivery from the vagina.Fertil Steril. 1983 Apr;39(4):490-3 PubMed
Ritschel WA. Targeting in the gastrointestinal tract: new approaches. Methods Find Exp CUn Pharmacol 1991;13:313-336. PubMed
Simon JA, Robinson DE, Andrews MC, Hildebrand JR 3rd, Rocci MLJr, Blake RE, Hodgen GD. The absorption of oral micronized PROGESTERONE : the effect of food, dose proportionality, and comparison with intramuscular PROGESTERONE . Fertil Steril 1993;60:26- 33.PubMed
Transvaginal PROGESTERONE : evidence for a new functional “portal system”flowing from the vagina to the uterus, Human Reprod 1999, Vol 5, No4 pp365-372 PubMed
Villanueva B, Casper RF, Yen SS. Intravaginal administration of PROGESTERONE : enhanced absorption after estrogen treatment. Fertil Steril. 1981 Apr;35(4):433-7. PubMed
Von Eye Corleta H, Capp E, Cardoso Ferreira MB. Pharmacokinetics of natural PROGESTERONE vaginal suppository. Gynecol Obstet Invest 2004;58:105-108.
Weckstein LN, Jacobson A, Galen D, Hampton K, Ivani K, Andres J. Improvement of pregnancy rates with oocytes donation in older recipients with the addition of PROGESTERONE vaginal suppositories. Fertl Steril 1993;60:573-575.